Unprecedented rates of substance abuse and mental illness have afflicted nearly every segment of our population in recent years. This intractable public health crisis has led healthcare professionals, policymakers, and other stakeholders to reexamine longstanding assumptions concerning the underpinnings of behavioral health and to consider novel (and controversial) interventions. Individuals with comorbid mental illness and Substance Use Disorder (SUD) encounter additional obstacles to effective care and are at significantly greater risk of poor health outcomes and other adverse events. This can be attributed, at least in part, to the prevalence of physical health conditions among those dually diagnosed with mental illness and SUD (Dickey et al., 2002). There are a host of other factors, however, that must be addressed to improve the health and overall wellbeing of this exceptionally vulnerable population.

By some indications, this should be an auspicious time to seek and to receive treatment for a behavioral health condition. According to the American Psychological Association, almost 90% of individuals surveyed repudiated stigma against persons with these conditions, and a comparable majority agreed they can improve with effective treatment (American Psychological Association, 2019). In addition, more Americans are enrolled in therapy than at any other point in our history (Ducharme, 2023). Nevertheless, we continue to bear witness to the most tragic manifestations of mental illness and substance use on a scale we would have considered unimaginable merely a decade ago. Deaths by suicide rose to a record level in 2022 (Centers for Disease Control and Prevention, 2023). Although deaths by overdose reached a record level in 2021 and declined slightly during the first half of 2022, they remained 50% higher than they were prior to the COVID-19 pandemic (Baumgartner & Radley, 2023). This paradoxical pairing of peak engagement in behavioral healthcare amid widespread tragedy illustrates the futility of approaches that rely solely on our healthcare system to remedy problems whose root causes remain deeply entrenched in enduring socioeconomic ills.
Authors Anne Case and Angus Deaton have documented the intersectionality of socioeconomic, political, and epidemiological trends that produce “deaths of despair” among broad segments of our population. These authors describe a confluence of developments that contributed to the first decrease in life expectancy in nearly a century (Case & Deaton, 2021). Their research affirms an a priori proposition that privations borne of pervasive unemployment, chronic and comorbid medical conditions, and other significant life challenges exact psychological tolls that frequently manifest as clinical depression, suicidality, and substance use. The individuals of interest to Case and Deaton include those who have been largely left behind by our “modern” (i.e., information) economy. They generally inhabit rural areas, have lower levels of educational attainment, and are broadly represented in the manual trades and at greater risk of physical injury and chronic medical conditions. They also proved especially susceptible to exploitation by pharmaceutical companies that peddled profoundly addictive opioid drugs and produced an epidemic of abuse whose ravages persist unabated (Case & Deaton, 2021).
These authors addressed certain ills unique to Appalachia and other rural regions, but their conclusions may be broadly applied to other populations deprived of fundamental necessities for a healthy and productive life irrespective of geography or other demographic factors. An extensive body of research has converged on a central conclusion concerning the relatively modest impact of healthcare on overall population health. By some estimates, “traditional” (i.e., clinical) care accounts for merely 20% of health outcomes. A considerably larger share may be attributed to the conditions in which people live, learn, work, and socialize (commonly known as Social Determinants of Health (SDoH) (Whitman et al., 2022). These findings have garnered attention from providers, payers, and policymakers alike, and they now inform a variety of approaches that aim to correct socioeconomic imbalances that perpetuate or exacerbate chronic illnesses. For instance, Harm Reduction and Housing First are leading evidence-based practices commonly employed among individuals with comorbid mental health and substance use conditions for whom conventional interventions have proven unsuccessful. One study employed a randomized controlled trial (RCT) to examine the differential effects of Housing First versus conventional (i.e., “abstinence-based”) care among a cohort of dually diagnosed individuals.
Those assigned to the experimental group received housing coupled with appropriate support services regardless of their perceived “readiness” for it. That is, their placement was not conditioned on abstinence, a remission of psychiatric symptoms, or other prerequisites that often present barriers to engagement among the most vulnerable and compromised populations. By contrast, participants assigned to the control group were required to abide by certain conditions in order to access or to maintain their housing as is customary within many programs and service settings. The investigation found members of the experimental group enjoyed greater housing stability and community tenure than members of the control group. Furthermore, experimental group participants did not exhibit a worsening of symptoms or deterioration in their overall health status despite ongoing substance use and disengagement from behavioral healthcare services (Tsemberis et al., 2004).
The foregoing findings do not suggest Housing First or similar interventions that facilitate individuals’ access to SDoH are panaceas. Interventions applied in a community-based context affect individuals to whom they are targeted and others in proximity. This was illustrated by another study that examined a Housing First approach applied within a congregate setting (i.e., one that included both individuals who used substances and those who abstained from them). Some study participants endorsed the flexibility and ease of access characteristic of the Housing First model, whereas others expressed ambivalence toward its application within congregate settings. The latter participants suggested continuing substance use by some individuals compromises the sobriety of others who aspire to abstinence (Kozloff et al., 2013). Other analyses suggest Housing First is effective at the individual level but has failed to yield appreciable decreases in homelessness overall, especially within certain regions or municipalities that tout its benefits (Knight, 2014). Some critics suggest Housing First and similar “low barrier” approaches are uniquely suited to a subset of the homeless population that makes frequent use of institutional care due to untreated health conditions whose symptoms are exacerbated by homelessness, but they claim a broader application of such approaches to all vulnerable persons is misguided insofar as it neglects the importance of treatment and service engagement in the recovery process (Eide, 2020).
As our nation continues to grapple with enduring epidemics of substance abuse and mental illness, our interventions will inevitably be guided by emerging evidence and myriad social, political, and economic factors. Those entrusted with the lives of the most vulnerable would do well to remember that suffering borne of illness and addiction is often indistinguishable from the pain we experience when our basic needs go unmet.
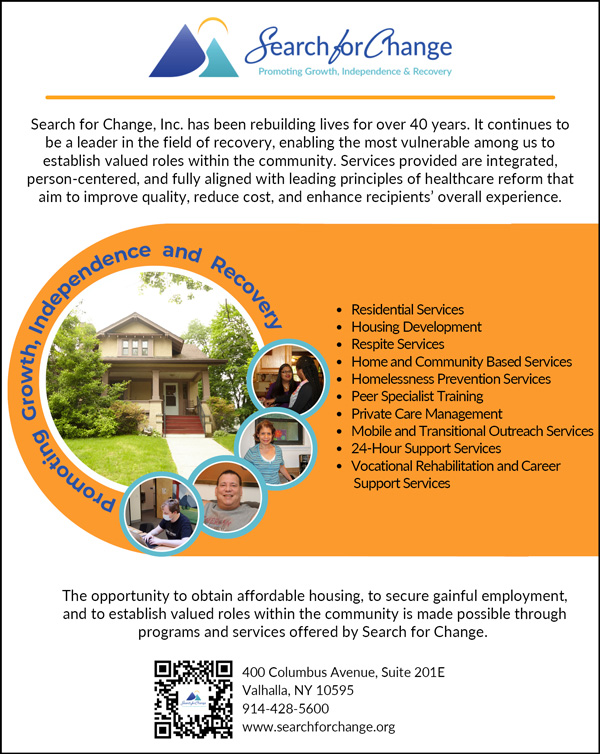
Ashley Brody, MPA, CPRP, is Chief Executive Officer of Search for Change, Inc. The author may be reached at (914) 428-5600 (x9228) or abrody@searchforchange.org.
References
American Psychological Association. (2019). Americans becoming more open about mental health. https://www.apa.org/news/press/releases/apa-mental-health-report.pdf
Baumgartner, J.C., & Radley, D.C. (2023, March 13). Overdose deaths declined but remained near record levels during the first nine months of 2022 as states cope with synthetic opioids. The Commonwealth Fund. https://www.commonwealthfund.org/blog/2023/overdose-deaths-declined-remained-near-record-levels-during-first-nine-months-2022-states
Case, A. & Deaton, A. (2021). Deaths of despair and the future of capitalism. Princeton University Press.
Centers for Disease Control and Prevention. (2023). Provisional suicide deaths in the United States, 2022. https://www.cdc.gov/media/releases/2023/s0810-US-Suicide-Deaths-2022.html
Dickey, B., Norman, S.T., Weiss, R.D., Drake, R.E., & Azena, H. (2002). Medical morbidity, mental illness, and substance use disorders. Psychiatric Services, 53(7), 861-867. https://ps.psychiatryonline.org/doi/full/10.1176/appi.ps.53.7.861
Ducharme, J. (2023, August 28). America has reached peak therapy. Why is our mental health getting worse? Time Magazine. https://time.com/6308096/therapy-mental-health-worse-us
Eide, S. (2020). Housing First and homelessness: The rhetoric and the reality. The Manhattan Institute. https://media4.manhattan-institute.org/sites/default/files/housing-first-and-homelessness-SE.pdf
Knight, H. (2014, June 30). A decade of homelessness: Thousands in S.F. remain in crisis. San Francisco Chronicle. https://www.sfchronicle.com/archive/item/A-decade-of-homelessness-Thousands-in-S-F-30431.php
Kozloff, N., Cheung, A.H., Ross, L.E., Winer, H., Ierfino, D., Bullock, H., & Bennett, K.J. (2013). Factors influencing service use among homeless youths with co-occurring disorders. Psychiatric Services, 64(9), 925-928. https://ps.psychiatryonline.org/doi/10.1176/appi.ps.201200257
Tsemberis, S., Gulcur, L., & Nakae, M. (2004). Housing First, Consumer Choice, and Harm Reduction for homeless individuals with a dual diagnosis. American Journal of Public Health, 94(4), 651-656. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1448313
Whitman, A., De Lew, N., Chappel, A., Aysola, V., Zuckerman, R., & Sommers, B.D. (2022). Addressing Social Determinants of Health: Examples of successful evidence-based strategies and current federal efforts. Assistant Secretary for Planning and Evaluation, Office of Health Policy. https://aspe.hhs.gov/reports/sdoh-evidence-review