Abstract
Background: Obsessive-Compulsive Disorder (OCD) affects over 3 million adults in the U.S. and is frequently accompanied by depression, anxiety, gastrointestinal issues, and sleep disturbances. Standard treatments, particularly selective serotonin reuptake inhibitors (SSRIs), often fall short—up to 40% of patients do not achieve sufficient relief. Less than 10% receive Exposure and Response Prevention (EXRP), the first-line behavioral therapy. This underscores the need for accessible, integrative, and personalized treatment approaches.
Methods: This study evaluated a multidisciplinary intervention combining EXRP, mindfulness-based therapy, expressive writing, cognitive restructuring, and lifestyle modifications. Forty participants (ages 17–51, mean = 6 weeks of treatment) received care at an intensive outpatient clinic. A collaborative team—including therapists, physicians, and specialists in psychiatry, endocrinology, and gastroenterology—administered treatment. Outcomes were assessed using the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS), Hamilton Depression Scale (HAM-D), and the Willoughby Fear Survey. Subgroup analyses explored differences by sex and age.
Results: Participants showed significant mental and physical health improvements. Y-BOCS scores declined by 57.2%, with 82% achieving >50% reduction. Depression symptoms dropped by 53.7%, and fear-based symptoms by 50.97%. Gains were consistent across age and sex groups. Adolescents showed the largest relative improvement. Self-reported sleep, GI distress, and tinnitus also improved.
Conclusion: This study highlights the effectiveness of an integrative, mind-body model for OCD and comorbid conditions. Writing-based therapies, embedded in multidisciplinary care, significantly reduced OCD and depression symptoms while improving overlooked physical symptoms. The findings support broader implementation of holistic, individualized care models in clinical settings.
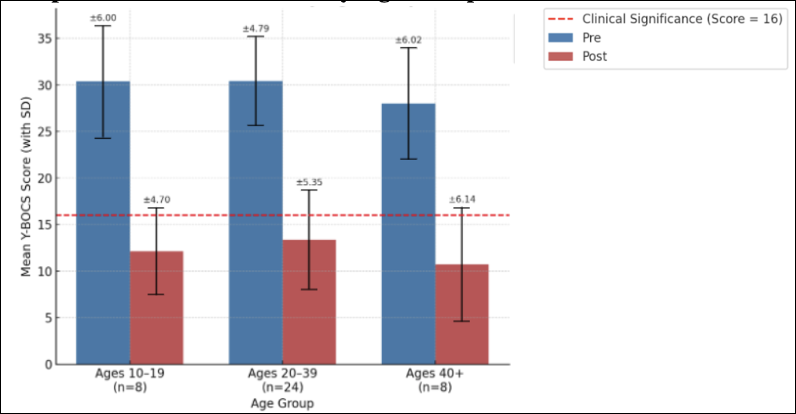
Graph 1: Y-BOCS reduction by Age Group
Introduction
Obsessive-compulsive disorder (OCD) is a chronic and often treatment-resistant mental health condition that significantly impairs daily functioning. Affecting more than three million adults in the United States (NIMH, 2023), OCD is frequently accompanied by comorbid depression and anxiety, both of which exacerbate functional decline and increase the risk of suicide (Fernández de la Cruz et al., 2017). According to the International OCD Foundation (2023), the average delay between symptom onset and treatment is approximately 11 years. During this time, comorbid conditions such as sleep disturbance, gastrointestinal dysfunction, and chronic stress responses often emerge (Cryan & Dinan, 2012; Riemann et al., 2020).
Despite the proven efficacy of Exposure and Response Prevention (EXRP), it remains vastly underutilized, reaching fewer than 10% of those diagnosed (Franklin et al., 2020). Selective serotonin reuptake inhibitors (SSRIs), the most common pharmacological treatment, yield only partial or inconsistent results in up to 40% of patients (Firth et al., 2019). These limitations are especially concerning for individuals with complex, comorbid presentations. The need for more comprehensive, biopsychosocial approaches has grown increasingly clear, as clinicians and researchers recognize the bidirectional interactions between mental and physical health.
At the Westwood Institute for Anxiety Disorders, we designed a multidisciplinary treatment framework that integrates behavioral therapy, expressive writing, mindfulness-based interventions, and physiological supports tailored to sleep and digestive health. This article presents outcome data from our intensive outpatient program, with a focus on treatment effectiveness and the practical benefits of a mind-body model.
Intervention and Methods
The treatment program included 40 participants (21 males, 19 females) between the ages of 10 and 54 (M = 27.5, SD = 10.2), all presenting with moderate to severe OCD, defined as having a baseline Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) score greater than 16. No participants were excluded based on comorbid conditions, allowing for a naturalistic assessment of real-world clinical complexity. The average duration of treatment was six weeks (range = 2 to 21 weeks), delivered in 3- or 6-hour intensive outpatient sessions, three to five days per week.
Each treatment plan was individualized based on clinical severity and patient availability. The integrative model included the following core components:
- Exposure and Response Prevention (EXRP): Delivered weekly by licensed therapists trained in evidence-based OCD treatment. EXRP sessions involved graduated exposure to distressing stimuli while patients practiced inhibiting ritualistic responses.
- Mindfulness-Based Therapy: Patients engaged in guided breathwork, body scanning, and cognitive diffusion techniques to develop distress tolerance and awareness of internal states.
- Expressive Writing: Participants completed structured journaling exercises and imaginal exposure scripts using detailed, first-person narratives that simulated feared scenarios. These were reviewed in session to promote cognitive reappraisal and emotional processing.
- Lifestyle Coaching: Tailored recommendations on nutrition, sleep hygiene, and digestive support were developed in collaboration with medical providers, including endocrinologists and gastroenterologists.
Results
Symptom changes were measured using the Y-BOCS for OCD severity and the Hamilton Depression Rating Scale (HAM-D) for depressive symptoms. Both instruments were administered pre- and post-treatment by trained assessors. On average, Y-BOCS scores declined by 57.2%, and 82% of participants demonstrated a reduction of greater than 50%. HAM-D scores showed a 53% mean reduction. These improvements were statistically and clinically significant (p < .01).
Participants also reported qualitative improvements in sleep, gastrointestinal function, and energy levels. Notably, symptom improvements were consistent across all age and sex groups. Adolescents (ages 10–19) exhibited particularly strong reductions in both OCD and depressive symptoms, as did adults over 40, a group often considered less responsive to behavioral therapy.
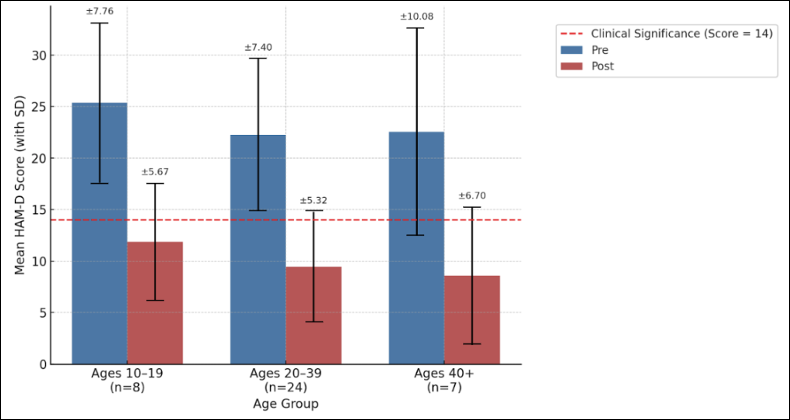
Graph 2: HAM-D reduction by Age Group
The Role of Expressive Writing
One of the most impactful tools in this model was guided expressive writing for imaginal exposures. Many individuals with OCD find it difficult to confront distressing thoughts through verbal dialogue alone. By writing about feared scenarios in detailed, first-person narratives, patients were able to process emotions more deeply and challenge their underlying beliefs. This form of imaginal exposure allowed patients to simulate feared outcomes, confront them with structured support, and gradually loosen the grip of obsessional thinking. In those with high intolerance of uncertainty, a common trait in OCD, this narrative approach proved particularly effective.
Why Integration Matters
What sets this model apart is its emphasis on treating the whole person. Rather than viewing OCD symptoms in isolation, we considered how chronic stress, inflammation, and dysregulation in systems like the gut-brain axis may reinforce emotional distress (Cryan & Dinan, 2012; Brander et al., 2019). This was especially important for patients with physical symptoms such as IBS or insomnia, which often exacerbated compulsions.
By collaborating with gastroenterologists and endocrinologists, we were able to create targeted interventions that addressed the physical dimensions of each patient’s presentation. Sleep routines, nutritional changes, and tailored mindfulness strategies helped stabilize physiological systems, which in turn reduced the severity of intrusive thoughts and compulsive behaviors.
Toward Scalable, Person-Centered Care
This intervention demonstrates that flexible, individualized care can be delivered in a scalable way. Patients attended daily intensive sessions tailored to their availability, and treatment components were adapted based on clinical need. Our findings suggest that integrative models, when properly coordinated, can produce substantial change within a relatively short timeframe. Most importantly, they offer hope to patients who have not responded to traditional care.
Limitations and Future Directions
This was a real-world clinical intervention, not a randomized controlled trial. While the symptom reductions were both significant and consistent, future research should examine long-term outcomes and explore how these models can be adapted for community-based and telehealth settings.
Conclusion
Effective treatment of OCD and comorbid depression requires more than symptom management. It requires addressing the full context of a person’s experience, including their emotional, physiological, and cognitive landscape. Our results suggest that integrative care models grounded in collaboration, personalization, and body-mind connection may offer a powerful path forward for patients with complex clinical needs.
Author Note
We have no known conflicts of interest. Correspondence concerning this article should be addressed via mail to Dr. Eda Gorbis, 921 Westwood Blvd., Suite 223, Los Angeles, California 90024, United States. Or by email to The Westwood Institute for Anxiety Disorders at thewestwoodinstitute@gmail.com.
Dr. Eda Gorbis is the Founder and Executive Director of the Westwood Institute for Anxiety Disorders in Los Angeles and a Clinical Assistant Professor (V) at the USC Keck School of Medicine. The Institute is often considered an intensive center of “last resort” for OCD, BDD, and related anxiety disorders. Dr. Gorbis has brought hundreds of treatment-resistant patients to full recovery through her integrative, team-based model. Her work has been featured on 20/20, 60 Minutes, and MTV’s True Life. She has delivered over 170 presentations globally on intensive treatment for OCD-spectrum disorders.
Alexander Gorbis holds a master’s in Clinical Psychology with an emphasis in Marriage and Family Therapy from Pepperdine University. His clinical background includes work with youth and neurodivergent adults. At the Westwood Institute for Anxiety Disorders, he supports complex OCD cases by conducting assessments and creating exposure-based treatments. He is currently pursuing a doctoral degree at The Chicago School for Professional Psychology.
Aanya Jajoo is the Clinic and Research Coordinator at the Westwood Institute for Anxiety Disorders. She will graduate from UCLA in 2025 with a major in Psychobiology and a minor in Brain and Behavioral Health. She brings experience as a clinical research assistant, behavior technician, and an advocate for mental health equity. Her focus is on OCD, anxiety, and culturally responsive care, particularly within South Asian and immigrant communities. This fall, she will begin the Ed.M. & M.A. program in Psychological Counseling at Teachers College, Columbia University.
Neha Mandava is a Clinical Coordinator at the Westwood Institute for Anxiety Disorders and a third-year undergraduate at UCLA majoring in Molecular, Cell, and Developmental Biology with a minor in Biomedical Research. Her academic and professional work integrates molecular research, mental health, and public health advocacy, with a focus on harm reduction–based health education. Neha aspires to pursue a career in medicine, aiming to deliver equitable, evidence-based care rooted in both scientific research and community engagement.
References
Brander, G., Pérez-Vigil, A., Larsson, H., & Mataix-Cols, D. (2019). Systematic review of environmental risk factors for obsessive-compulsive disorder: A proposed roadmap from association to causation. Neuroscience & Biobehavioral Reviews, 107, 446–462. https://doi.org/10.1016/j.neubiorev.2019.09.005
Cryan, J. F., & Dinan, T. G. (2012). Mind-altering microorganisms: The impact of the gut microbiota on brain and behaviour. Nature Reviews Neuroscience, 13(10), 701–712. https://doi.org/10.1038/nrn3346
Fernández de la Cruz, L., Rydell, M., Runeson, B., D’Onofrio, B. M., Brander, G., Ruck, C., … & Mataix-Cols, D. (2017). Suicide in obsessive–compulsive disorder: A population-based study of 36,788 Swedish patients. Molecular Psychiatry, 22, 1626–1632. https://doi.org/10.1038/mp.2017.10
Firth, N., Meeten, F., & Rees, C. (2019). Understanding the barriers to accessing specialist support for obsessive-compulsive disorder: A qualitative study. BMC Psychiatry, 19(1), 1–12. https://doi.org/10.1186/s12888-019-2343-4
Franklin, M. E., Sapyta, J., Freeman, J. B., Khanna, M., Compton, S., Almirall, D., … & Foa, E. B. (2020). The Pediatric Obsessive Compulsive Treatment Study II: Randomized controlled trial of family-based cognitive behavioral therapy and medication. Journal of the American Academy of Child & Adolescent Psychiatry, 60(2), 197–207. https://doi.org/10.1016/j.jaac.2020.03.019
International OCD Foundation. (2023). OCD Facts. https://iocdf.org/about-ocd/
National Institute of Mental Health. (2023). Obsessive-Compulsive Disorder. https://www.nimh.nih.gov/health/statistics/obsessive-compulsive-disorder-ocd
Riemann, D., Krone, L. B., Wulff, K., & Nissen, C. (2020). Sleep, insomnia, and depression. Neuropsychopharmacology, 45, 74–89. https://doi.org/10.1038/s41386-019-0411-y










