The current state of value-based care (VBC) can be characterized by the challenges many organizations face as they attempt to obtain and operationalize their value-based agreements. Stakeholders are trying to work through practical solutions for organizations representing services that weren’t initially considered in the original Accountable Care Organizations (ACO) models. These types of provider organizations include healthcare at-home services and behavioral health services. Perhaps the most significant challenge for these providers is finding a reimbursement model that meets their set of services and captures the value that those services produce.
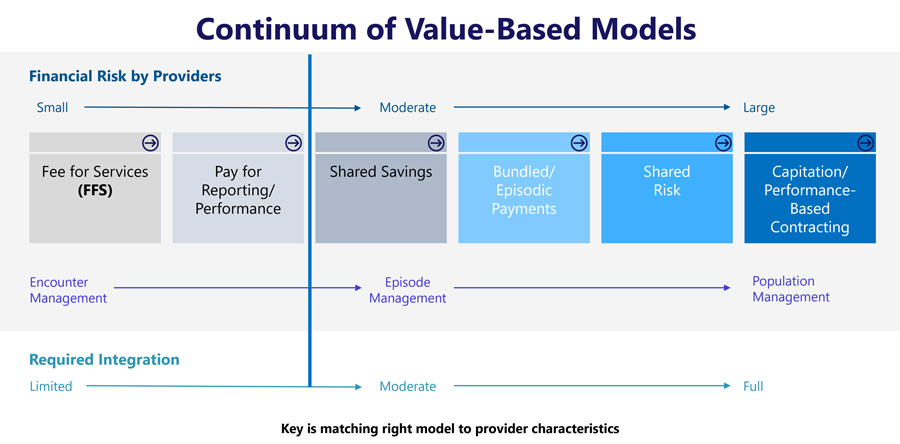
Many organizations want to move toward risk-based arrangements and away from pay-for-performance programs but can’t find the right model for their services. Before establishing or evolving your value-based model, it is imperative to determine your organization’s “best fit” placement along the continuum. For those organizations that treat their patients in discrete episodes, bundled payments can be the right fit across the VBC continuum.
A common challenge across the continuum is translating clinical models into a measurable, implementable structure consistent with the VBC contract. This may sound logical and obvious, but it is inconsistent with how most organizations operate under a transactional, fee-for-service structure. Transitioning to a population-centered program from an individual care program driven by the fee-for-service world is a more significant change than many organizations realize.
One critical area for modifying the clinical model and workflows is to drive data reporting needs. Data analytic needs – in terms of both claims’ ingestion and measurement of outcomes – are essential to substantiate the value-based contract and often are not a core competency for provider organizations. In managed Medicaid environments, there typically is a need to both track encounters and measure outcomes. Despite the primary focus of value-based care as outcome-focused care, the translation to Medicaid requirements is still in transition, and thus, tracking and measuring both encounters and outcomes is important.
The promise that value-based care can bring – whether clinical (e.g., better patient care) or financial (e.g., increase in revenue or margin) – is still evolving, but some basic practices are critical.
- Movement to a more programmatic clinical model while maintaining the care needed for a specific patient is important for your value-based program.
- Focusing on your program differentiators and how they can positively affect your outcomes is critical to operationalizing.
- Workflows can change, and measuring outcomes and leading indicators (including process measures) is critical.
- Developing an analytic strategy is necessary for VBC arrangements and must be a priority. When scaling your efforts, the “heroic efforts” of a few individuals to create reports and manipulate the data becomes difficult.
- Tracking encounters and reportable activity bridges the transition gap from fee-for-service to risk-based arrangements, especially for Medicaid.
- Lastly, understanding the technology to implement your value-based contract is critical. For example, does the claims system have the capability to support a case rate or bundled payment? Alternatively, is there another code available that can be used as a proxy to file claims?
Creative approaches to specialized provider (e.g., healthcare at home and behavioral health) reimbursement and coding initiatives have been initiated for value-based care programs. For example, a group of services now performed at home for a given patient differs greatly from a single home care visit. Given the challenges of provider availability in behavioral health care, measuring access to care becomes an important outcome.
Many health plans have reservations about proceeding with value-based care, not because they don’t support the initiative but because they are concerned about implementing and managing these programs. Creating a structure that doesn’t create extensive management and reporting efforts goes a long way to clear the path to the value-based care Promised Land.
For morning information about CWH Advisors, visit www.cwhadvisors.com.






