Many behavioral health providers around the country are trying to establish and implement alternative payment models in hopes of focusing on reducing costs and improving outcomes, especially for more acute patients. However, many states and health plans lag, creating a disincentive for already scarce behavioral health resources. There have been many articles and studies directed at understanding the continued shortages of providers, but payment solutions have not been addressed sufficiently. With potential looming cuts to Medicaid, access to mental health care will mostly likely continue to trend in a less-than-desirable trajectory. So, what can we do to trend in a better direction?
An example of the inherent structural problems was explained by the 2024 committee commissioned by CMS, stating in their findings, “the median state Medicaid program paid psychiatrists 81 percent of the Medicare fee schedule for psychiatrists (Zhu et al., 2023). In Medicaid, capitation rates are based on historical FFS Medicaid spending levels that typically occurred under a benefit structure that frequently imposed strict limits on behavioral health services. Therefore, the capitation rates are inconsistent with the benefit designs that define the responsibilities of the Medicaid MCOs.1
How do we get around these limitations and provide needed access to care? There are providers who are delivering innovative, longitudinal programs, including housing, Social Determinants of Health (SDOH), and case management services, which are positively impacting mental health and cost outcomes. How can they afford to provide these services? Some of these providers have worked with progressive MCOs to implement value-based care arrangements at typically bundled rates that include these services. Not surprisingly, the outcomes are much better than national trends.
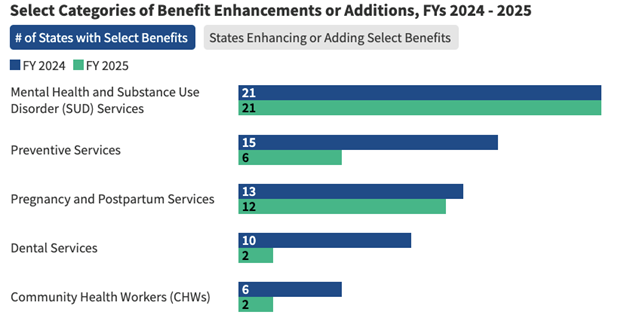
Maybe the solution lies in a gradual implementation approach where case management is compensated for helping, especially co-occurring patients stay in recovery and get better. In many states, Medicaid doesn’t typically compensate for case management or care coordination, and if they do, it’s for patients with serious mental illnesses and/or specific populations like pregnant women. Benefit enhancements are being implemented in many states, including addressing SDOH needs.2 There are also benefit changes regarding Community Health Workers who may perform culturally appropriate health promotion and education, care coordination, and help accessing medical and non-medical services. The table depicts how many states have recently added these new benefits.
Incentives and compensation are at the heart of providing the care that is needed to reduce costs and change the curve. Refocusing on improving outcomes is best for the patient and for the industry. Consideration of case management/ care navigation as a starting point may help to simplify the change and help mitigate the provider shortage issue and access to care.
Jeff Gershman is CEO of Square Medical Group. Janie Tremlett is Partner at CWH Advisors.
Footnotes
- Expanding Behavioral Health Care Workforce Participation in Medicare, Medicaid, and Marketplace Plans Copyright National Academy of Sciences. https://www.commonwealthfund.org/publications/explainer/2022/sep/behavioral-health-care-us-how-it-works-where-it-falls-short
- Annual KFF survey of state Medicaid officials conducted by Health Management Associates, October 2024
Sources





