It is hard to separate gastric distress from psychological distress due to the connection between the brain and the gut. One can lead to the other, and ultimately, while medications can support managing physiological symptoms, psychological interventions may be needed to reduce ongoing symptoms most effectively. The American Psychological Association published an article in April 2025 relating the impacts of the gut microbiome on presentations of anxiety and depression (Abramson, 2025). Abramson notes that there is a growing field of “gastropsychologists” who focus on the connection between the brain and gut to treat the common co-occurrence of mental illness and gastrointestinal symptoms. The prevalence of anxiety and depression among those with gastric distress suggests that cognitive behavioral therapy (CBT) and mindfulness can help moderate symptoms.
Mood and anxiety disorders commonly co-occur among those with gastrointestinal disorders, with women being approximately twice as likely to seek treatment for IBS as men and being more likely to experience co-occurring depression and anxiety (Kim & Kim, 2018; Naliboff, Frese, & Rapgay, 2007; Tarar, Farooq, Zafar, 2023; Staudacher et al., 2023). Symptoms of IBS can feel embarrassing or even shameful, which further contributes to symptoms of depression, anxiety, and detachment from or anger towards one’s body (Geller, Levy, & Avitsur, 2024).
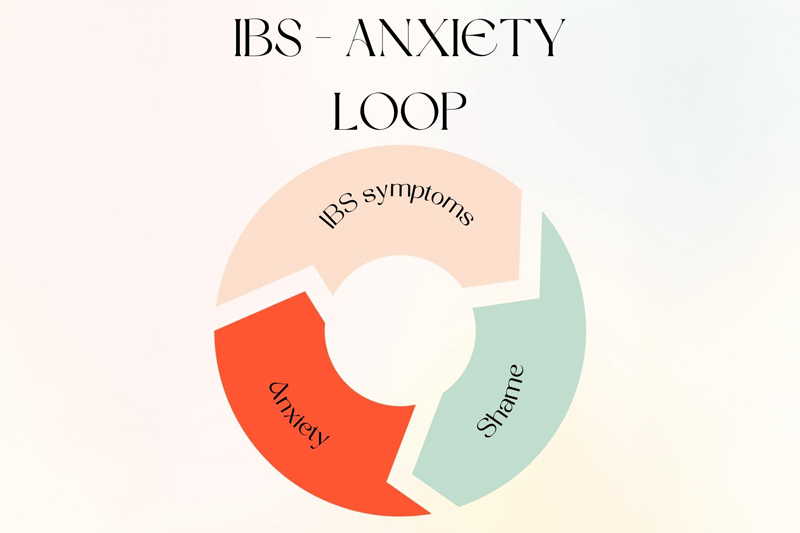
Stomach pain, dizziness, nausea, and indigestion are common somatic complaints associated with anxiety (Gelenberg, 2000; Geller, Levy, & Avitsur, 2024; Kolacz & Porges, 2018). While IBS is a disease of the gut, anxiety can exacerbate symptoms due to its induction of somatic symptoms. The somatic symptoms of anxiety can cause a feedback loop of anxiety, IBS symptoms, embarrassment, and worsened IBS symptoms (Geller et al, 2024). The National Institute of Diabetes and Digestive and Kidney Diseases recommends that IBS be managed with medical, mental, and behavioral health interventions.
Vagus Nerve and the Gut
In the 1990s, Stephen Porges, PhD, developed the Polyvagal Theory, which has also contributed to the development of somatic therapy modalities to treat psychological distress. The vagus nerve extends from the brain to the gut, serving as the “mind-gut connection” (Özçağlayan et al., 2020). This nerve plays a role in regulating the autonomic nervous system, also known as subconscious physiological responses, including heartbeat, respiration, stress response, and digestion. The autonomic nervous system is considered to have two primary branches: the parasympathetic nervous system, which maintains a rested state, and the sympathetic nervous system, which is activated during times of stress (Porges, 2011). Polyvagal Theory’s biggest strength is its accepted role in mobilizing the parasympathetic nervous system. It is understood that a functioning vagus nerve acts as a “brake” on the body’s stress response and returns it to a restful state. Somatic therapists and polyvagal theorists recommend “vagal toning” to improve our responses to stress.
The APA and NIH already recognize the mind-gut link and recommend mental health approaches in addition to medical IBS management for those struggling with both IBS and anxiety or mood disorders (Abramson, 2025; National Institute of Diabetes and Digestive and Kidney Diseases). While overarching research has not shown that the vagus nerve causes or mitigates symptoms of irritable bowel syndrome (Özçağlayan et al., 2020), some theorists posit that polyvagal theory can explain the development of disorders, such as irritable bowel syndrome and fibromyalgia, following an acute trauma (Kolacz & Porges, 2023). Additionally, mindfulness may be an effective treatment strategy due to its innervation and toning of the vagus nerve (Marchand, 2014; Lucas, Keplin, Porges, & Rejeski, 2016; Gerritson & Band, 2018; Kalyani et al., 2011; Brown, Ryan, & Creswell, 2007).
A systematic review of the research suggested that polyvagal stimulation can be helpful in managing IBS symptoms (Veldman, Hawinkels, & Keszthelyi, 2025). This review concluded that electrostimulated vagal nerve toning may reduce IBS symptoms by reducing inflammation. Additional research into the impacts of the vagus nerve on IBS and gut health is still needed, but Polyvagal Theory may offer additional treatment mechanisms that can help manage both IBS symptoms directly and anxiety.
Polyvagal Exercises for IBS
There is preliminary evidence suggesting that there are some exercises to support vagal tone and reduce stress and improve physical health. Some evidence-based recommendations that could support with managing anxiety-induced IBS symptoms are:
- Cold stimulation: A common DBT distress tolerance is to splash cold water on the face or fully immerse yourself in cold water. Research suggests that cold stimulation not only reduces stress but also improves cardiovascular function via vagal nerve toning (Jungmann et al., 2018).
- Mindfulness and mindful movement: Evidence shows that vagal toning is the physiological explanation for the efficacy of meditation, deep breathing, yoga, and tai chi in reducing stress. These practices have been demonstrated to reduce inflammation, improve cardiac function, reduce symptoms of mood disorders, anxiety, and trauma-related stress, and improve cognition and attention (Gerritson & Band, 2018; Keefer & Blanchard, 2001; Lucas, Kelpin, Porges, & Rejeski, 2011; Brown, Ryan, & Creswell, 2001).
- “Om chanting”: There is preliminary evidence that chanting ‘om’ deactivates the limbic system (sometimes called the emotional center of the brain) and the amygdala, which is a brain region activated in response to stressors (Kalyani et al., 2011). The authors of the “om chanting” study suggest that these effects are mediated by the auricular branches of the vagus nerve in the ears, rather than by stimulating the nerve via the throat (such as in gargling, which is a common polyvagal practice).
Conclusion
In sum, while research on the vagus nerve and its role in managing IBS, anxiety, and depression is still emerging, the existing evidence highlights a promising link between vagal tone and symptom relief. Approaches such as mindfulness, cold stimulation, and somatic practices may offer accessible ways to strengthen this connection, supporting both physical and mental health. As the field of gastropsychology grows, continued exploration of polyvagal theory and vagal toning exercises could provide more holistic, integrative treatment options for those managing the complex overlap of gastrointestinal and psychological distress.
Skye Dina Ross, LCSW, MPH, is a Therapist in Private Practice. For more information, email skye@skyerosstherapy.com and visit skyerosstherapy.com.
References
Abramson, A. (2025). The Undeniable Mind-Body Connection in Gastrointestinal Health. American Psychological Association. Retrieved from https://www.apa.org/topics/health-care/gastrointestinal-health?utm_source=linkedin&utm_medium=social&utm_campaign=apa-healthcare&utm_content=gastrointestinal-health
Brown, K.W., Ryan, R.M., & Creswell, J.D. (2007). Mindfulness: Theoretical Foundations and Evidence for its Salutary Effects. Psychological Inquiry, 4, 211-237. https://doi.org/10.1080/10478400701598298
Fülling, C., Dinan, T.G., & Cryan, J.F. (2019). Gut Microbe to Brain Signaling: What Happens in Vagus… Neuron,101(6), 998-102. Science Direct
Geller, S., Levy, S., & Avitsur, R. (2024). Psychological distress in individuals with irritable bowel syndrome: The role of body image and self-criticism. Health Psychol Behav Med, 12(1). https://doi.org/10.1080/21642850.2024.2334466
Gerritson, R.J.S., & Band, G.P.H. (2018). Breath of Life: The Respiratory Vagal Stimulation Model of Contemplative Activity. Frontiers in Human Neuroscience, 12, 397. https://doi.org/10.3389/fnhum.2018.00397
Jungmann, M., Vencatachellum, S., Ryckeghem, D.V., & Vögele, C. (2018). Effects of Cold Stimulation on Cardiac-Vagal Activation in Healthy Participants: Randomized Controlled Trial. JMIR Formative Research, 2(2), https://doi.org/10.2196/10257
Kalyani, B. G., Venkatasubramanian, G., Arasappa, R., Rao, N. P., Kalmady, S. V., Behere, R. V., Rao, H., Vasudev, M. K., & Gangadhar, B. N. (2011). Neurohemodynamic correlates of ‘OM’ chanting: A pilot functional magnetic resonance imaging study. International Journal of Yoga, 4(1), 3–6. https://doi.org/10.4103/0973-6131.78171 ResearchGateIJIP
Keefer L., & Blanchard E.B. (2001). The effects of relaxation response meditation on the symptoms of irritable bowel syndrome: results of a controlled treatment study. Behavior Research and Therapy, 39(7), 801–811. https://doi.org/10.1016/s0005-7967(00)00078-4
Kolacz, J., & Porges, S.W. (2018). Chronic Diffuse Pain and Functional Gastrointestinal Disorders After Traumatic Stress: Pathophysiology Through A Polyvagal Perspective. Frontiers in Medicine, 5, 145. https://doi.org/10.3389/fmed.2018.00145
Lucas, A.R., Klepin, H.D., Porges, S.W., & Rejeski, W.J. (2016). Mindfulness-Based Movement: A Polyvagal Perspective. Integr Cancer Ther, 17(1), 5-15. https://doi.org/10.1177/1534735416682087
Marchand, W.R. (2014). Neural Mechanisms of Mindfulness and Meditation: Evidence from Neuroimaging Studies. World J Radiol, 6(7), 471-479. https://doi.org/10.4329/wjr.v6.i7.471
Mayer, E.A., Ryu, H.J., & Bhat, R.R. (2023). The Neurobiology of Irritable Bowel Syndrome. Molecular Psychiatry, 28, 1451-1465. https://doi.org/10.1038/s41380-023-01972-w
Naliboff, B.D., Frese, M.P., & Rapgay, L. (2007). Mind/Body Psychological Treatments for Irritable Bowel Syndrome. Evid Based Complement Alter Med, 5(1), 41-50. https://doi.org/10.1093/ecam/nem046
Özçağlayan, O., Özçağlayan, T.I.K., Doğru, M., & Mete, R. (2020). Vagus Nerve Assessment Via Ultrasonography in Irritable Bowel Syndrome. Are There Any Changes of Dimension in the Vagus Nerve? Turk J Gastroenterol, 31(7), 503-507. https://doi.org/10.5152/tjg.2020.19353
Porges, S. (2011). The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-regulation. New York, NY: W.W. Norton & Company, Inc.
Porges, S.W. (2022). Polyvagal Theory: A Science of Safety. Frontiers in Integrative Neuroscience, 16. https://doi.org/10.3389/fnint.2022.871227
Staudacher, H.M., Black, C.J., Teasdale, S.B., Mikocka-Walus, A., & Keefer, L. (2023). Irritable Bowel Syndrome and Mental Health Comorbidity – Approach to Multidisciplinary Management. Nat Rev Gastroenterol Hepatol, 1-15. https://doi.org/10.1038/s41575-023-00794-z
Tarar, Z.I., Farooq, U., Zafar, Y. et al. (2023). Burden of anxiety and depression among hospitalized patients with irritable bowel syndrome: a nationwide analysis. Ir J Med Sci, 192, 2159–2166. https://doi.org/10.1007/s11845-022-03258-6
Treatment for Irritable Bowel Syndrome: How do doctors treat IBS? (n.d.). National Institute of Diabetes and Digestive and Kidney Diseases. Accessed 8/10/2025. https://www.niddk.nih.gov/health-information/digestive-diseases/irritable-bowel-syndrome/treatment
Veldman, F., Hawinkels, K., & Keszthelyi, D. (2025). Efficacy of Vagal Nerve Stimulation in Gastrointestinal Disorders: A Systematic Review. Gastroenterology Report, 13. https://doi.org/10.1093/gastro/goaf009




