Psychotropic medication nonadherence in populations with Serious Mental Illness (SMI) can lead to inadequate symptom control, reduced treatment effectiveness, significant relapse risk, and increased risk of death (Semahegn, 2020). Nonadherence to medication also results in increased healthcare utilization. Individuals who do not adhere to their prescribed medication regimen require more frequent visits to healthcare providers, emergency department visits, and hospitalizations (Ascher-Svanum et al., 2006). This places an increased burden on the individual, their families, and healthcare systems. Studies (Walsh et al., 2019; Phan, 2016) have found that individuals who are non-adherent to medication are more likely to require hospitalization due to worsening symptoms, increased functional impairment, or the inability to manage their condition in the community.

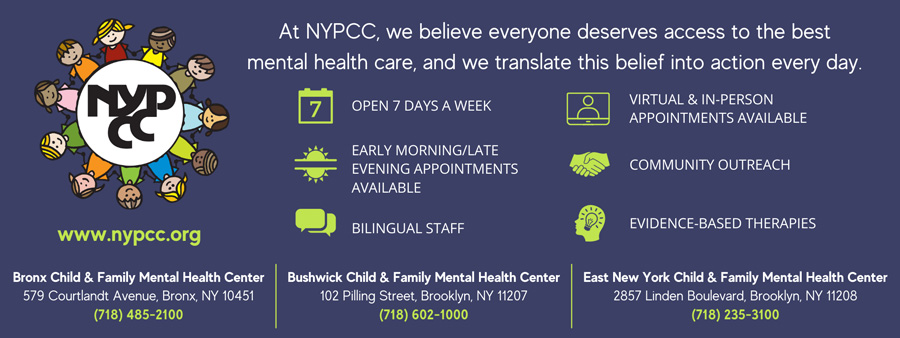
As one of the largest providers of outpatient mental health services in New York State, New York Psychotherapy and Counseling (NYPCC) collaborates with thousands of New Yorkers experiencing serious mental illnesses such as schizophrenia, schizoaffective disorder, and bipolar disorder. As a part of our commitment to improving the quality of care for NYC’s underserved populations, NYPCC has an intrinsic interest in reducing instances of non-adherence. Our therapists, psychiatrists, and nurse practitioners continuously monitor medication adherence among all our patients and intervene to increase adherence.
Improving medication compliance in people with serious mental illness can be challenging, as individuals may experience side effects, forget to take their medication, or resist treatment due to personal beliefs or concerns. However, there are several strategies that strengthen medication adherence and are essential for assisting patients to achieve their treatment goals.
The Therapeutic Alliance
At NYPCC, we emphasize the importance of a good therapeutic alliance in addressing potential adherence issues. A good therapeutic alliance fosters trust and promotes open communication between the patient and the clinician. Patients are more likely to share their concerns, doubts, and challenges related to medication adherence when they feel comfortable and trust their provider. This open dialogue allows the provider to gain insights into the patient’s adherence behaviors and potential barriers.
Patients may not always be forthcoming about their struggles with medication adherence due to fear of judgment or other reasons. A strong therapeutic alliance helps providers assess adherence more accurately by creating a safe and non-judgmental environment. Patients are more likely to disclose any non-adherence or difficulties they face, enabling providers to gather comprehensive information about their medication-taking behaviors. A good therapeutic alliance also allows clinicians to understand the patient’s motivations, beliefs, and attitudes toward medication. By exploring the patient’s perspectives, providers can identify potential factors that may influence medication adherence, such as concerns about side effects, doubts about the medication’s effectiveness, or conflicting beliefs about healthcare. Understanding these factors helps tailor interventions to address the specific needs and concerns of the patient. Finally, a strong therapeutic alliance promotes collaborative decision-making, where providers and patients work together to develop strategies that fit the patient’s lifestyle, preferences, and capabilities.
Tailoring Treatment Plans
NYPCC clinicians also tailor treatment plans to meet an individual’s needs through collaboration and shared decision-making. When patients actively participate in the treatment planning process and feel that their opinions and preferences are valued, they are more likely to adhere to the prescribed medication regimen. By shaping the treatment plan to the individual’s needs, clinicians can choose a route of medication delivery that minimizes side effects and enhances tolerability. This personalized approach improves the individual’s overall treatment experience and reduces the likelihood of discontinuation or non-adherence due to intolerable side effects. When treatment plans are based on an individual’s needs, it increases their satisfaction with the treatment and fosters a sense of engagement in their own care. By involving patients in the decision-making process and considering their preferences, clinicians empower individuals to take an active role in managing their condition. This increased engagement can lead to better treatment adherence, improved trust in the provider, and a higher overall satisfaction with the treatment experience.
Family Involvement
Involving family members or key persons in the care of a patient and providing them with psychoeducation can have several medication adherence benefits. Family members and key persons play a vital role in providing emotional and practical support to patients. By involving them in the care and treatment process, patients have access to a strong support system that can positively impact medication adherence. Family members can offer reminders, assistance with medication administration, and help create a structured routine around medication-taking, thereby increasing adherence. In certain cases, patients may have difficulty managing their medication independently due to cognitive impairments, physical limitations, or other factors. Involving family members or key persons can ensure proper medication supervision and reduce the risk of missed or incorrect doses. This involvement enhances medication adherence, particularly for patients who require assistance with complex medication regimens. Involving family members in psychoeducation provides them with a better understanding of the patient’s condition, treatment plan, and the role of medications. This shared knowledge promotes effective communication between the patient, family members, and clinicians. It allows for informed discussions, shared decision-making, and the development of strategies to overcome potential barriers to medication adherence. Family members or key persons who are actively involved in the patient’s care can provide valuable insights into adherence challenges that the patient may be facing. They may notice patterns of non-adherence, identify barriers, or observe changes in the patient’s behavior that could impact medication adherence. This information can help clinicians develop targeted interventions and support strategies to address those challenges. It’s important to note that involving family members or key persons should be done with the patient’s consent and in line with their preferences and privacy considerations.
Additional Adherence Strategies
Providing comprehensive education about the benefits of medication, the specific condition being treated, and the importance of adherence are valuable strategies to improve compliance. Helping individuals understand how their medication works, what to expect, and how it can improve their quality of life helps address concerns or misconceptions patients may have. Clear communication is key to adherence. Fostering open and honest communication by encouraging individuals to ask questions, express their concerns, and discuss any challenges they may face in adhering to their medication regimen is crucial to support adherence. Providers actively listen, provide clear instructions, offer support, and address key information about medications (what, why, when, how, and how long). Some individuals are hesitant to take medication due to concerns about side effects or perceived lack of efficacy. To address these concerns, prescribers must take time to discuss potential side effects, their likelihood, and ways to manage them. If side effects are interfering with adherence, prescribers work with the individual to explore alternative medications or adjunctive treatments.
NYPCC prescribers foster adherence by simplifying medication regimens as much as possible by minimizing the number of medications and reducing dosing frequency whenever appropriate. A simpler regimen is easier to remember and follow, reducing the chances of missed doses. Switching to a Long-Acting Injectable (LAI) medication is also a useful strategy to improve medication compliance in individuals who have difficulty adhering to oral medications or experience frequent relapses despite treatment. Therapists complement medication treatment with psychosocial interventions, such as therapy, counseling, or support groups. These interventions help individuals develop coping strategies, enhance motivation, and provide a holistic approach to managing their condition. NYPCC therapists also help individuals implement reminder systems to help remember to take medications as prescribed. These aids include alarms, pill organizers, smartphone apps, or setting medication-taking routines. Additionally, therapists encourage individuals to consider involving family members or trusted individuals who can provide support and reminders.
Medication compliance is a shared responsibility between individuals, the treatment team, and support networks. By implementing these strategies and fostering a collaborative approach, it is possible to improve medication adherence and enhance the treatment outcomes of people with serious mental illness.
Jonathan Keigher, PhD, is Vice President, Chief Clinical and Compliance Officer, at New York Psychotherapy and Counseling Center. To contact Jonathan, email JKeigher@nypcc.org, call (212) 729-1080, and visit the New York Psychotherapy and Counseling Center at www.nypcc.org.
References
Ascher-Svanum, H., Faries, D. E., Zhu, B., Ernst, F. R., Swartz, M. S., & Swanson, J. W. (2006). Medication adherence and long-term functional outcomes in the treatment of schizophrenia in usual care. The Journal of clinical psychiatry, 67(3), 453–460.
Phan, S. V. (2016). Medication adherence in patients with schizophrenia. The International Journal of Psychiatry in Medicine, 51(2), 211–219.
Semahegn, A., Torpey, K., Manu, A., Assefa, N., Tesfaye, G., & Ankomah, A. (2020). Psychotropic medication non-adherence and its associated factors among patients with major psychiatric disorders: a systematic review and meta-analysis. Systematic reviews, 9(1), 17.
Walsh, C. A., Cahir, C., Tecklenborg, S., Byrne, C., Culbertson, M. A., & Bennett, K. E. (2019). The association between medication non-adherence and adverse health outcomes in ageing populations: A systematic review and meta-analysis. British journal of clinical pharmacology, 85(11), 2464–2478.