Like many people who struggle with mental illness, Helise withdraws and isolates herself when she feels overwhelmed. While alone and shut in, she found herself ruminating about her thoughts and feelings, this pattern only made her feel worse. Feeling isolated and uncertain about what to do, Helise needed help. She was fortunate to find it with Bridgeway Behavioral Health Services, but many individuals with mental illness aren’t so lucky.
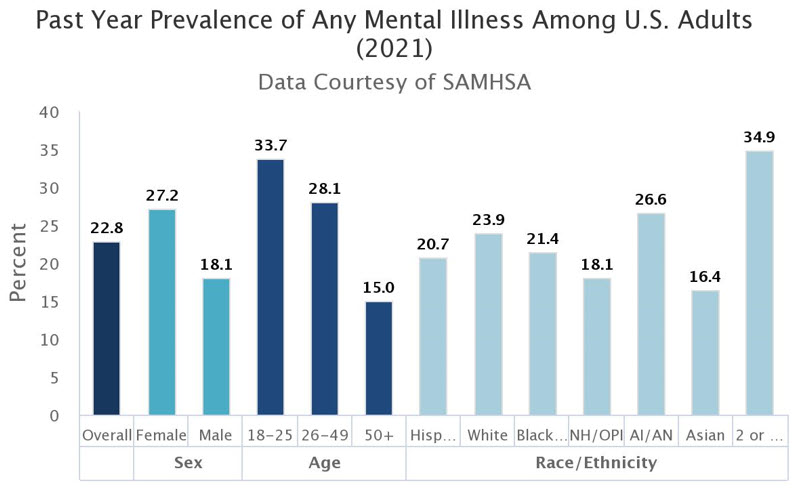
Poor mental health and diagnosed mental health illness affect millions of US adults: approximately one in five Americans (53 million) experience a mental illness (Center for Disease Control and Prevention (CDC)).
While there is no single cause for mental illness, the root cause varies from traumatic experiences, an imbalance in brain chemistry, and significant struggles associated with other medical/health conditions and life in general (CDC, World Health Organization). Mental illness can be debilitating—interfering with quality of life, leading to loneliness and isolation, and tragically, can even result in death (National Alliance on Mental Illness (NAMI), California). People do not always get care when needed; in fact, less than half (46%) of individuals with mental health concerns are currently receiving care (NAMI-A). When people do seek professional help, they often have to wait several months to see a professional, resulting in additional suffering and increased daily challenges.
There are many proven and effective behavioral and pharmacological treatments for mental illness; however, access to timely care is often hindered. In recent years, mental health concerns and the need for mental health care have been outpacing the availability of mental care professionals and behavioral health specialists. To further complicate matters, primary care providers lack the training, expertise, and time to properly treat mental health conditions.
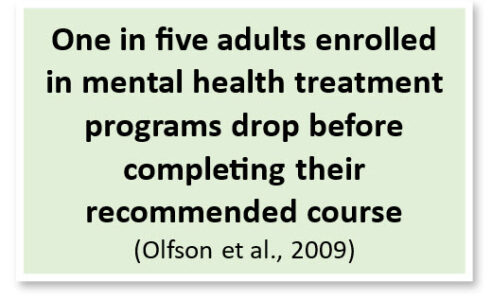
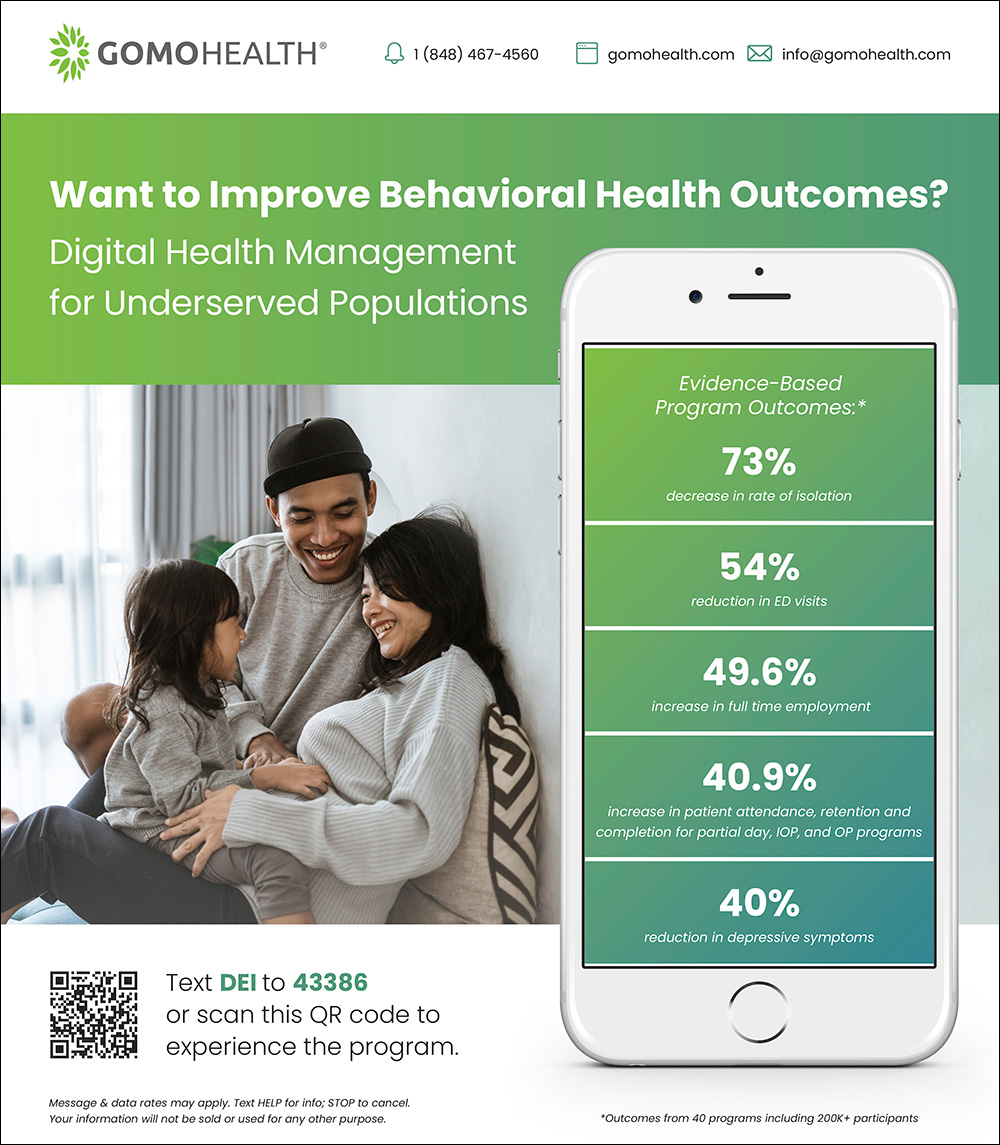
Behavioral treatment options typically range from one-on-one or group care delivered through outpatient or residential programs. While these programs can be incredibly effective, the type and amount of care delivered is typically limited to the time in-session and rarely includes out-of-session support. Thus, the structure of behavioral therapy may leave patients feeling lost or unclear about how to implement treatment recommendations outside of the in-person care delivery setting. Fortunately, there are many innovative solutions, such as those designed and offered by GoMo Health, addressing these care gaps and improving adherence to treatment and treatment outcomes.
Every Day Matters: A Combined In-Person and Remote Care Coordination Program
A little more about Helise, who was first introduced at the beginning of this article: Helise was diagnosed with borderline personality disorder and struggled to leave her house. This, of course, presented challenges with attending her partial-day treatment program. Her condition became so prohibitive that her most frequent personal interaction was with the pizza delivery person, who eventually began bringing her cat food and litter so she could properly care for her pet.
Watch Helise’s full story:
Bridgeway, a New Jersey-based psychiatric rehabilitation services provider, recognized a pattern with Helise and other members, who would show up initially for their in-person group sessions and then taper off their regular attendance. Patients shared a variety of reasons for the drop off—they began to feel better and didn’t think additional care was needed; the pending sessions were overwhelming to consider attending even the night before, let alone the day of; or they gave in to lack of confidence and simply didn’t show. For many patients who didn’t show, they didn’t recognize the impact it had on the other members of the group. They gave in to their lack of self-confidence which made it difficult to engage in treatment.
The Bridgeway leadership and staff knew that patients could only improve if they came to group sessions and followed treatment recommendations—in person and at home. The team at Bridgeway was certain that if they could address the hesitation to come to program in the moment, they’d have a higher likelihood of people regularly attending in person.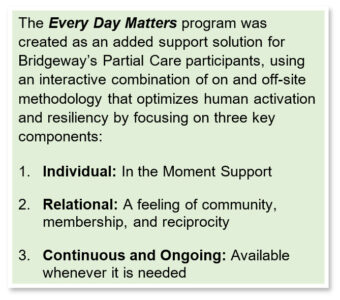
So was born the Bridgeway Every Day Matters program. This program, created and operated by GoMo Health, was designed to leverage the membership concept, empowering Bridgeway patients to be healthy, positive members of society and maintain that mindset. The goal was to create a sense of community, to motivate patients to show up, engage in, and follow their treatment plan and recommendations, and to transform the Bridgeway Day Program into a ‘Lifestyle Program.’ This was achieved by using technology-enabled messaging to provide intervention content at the right time, reinforce target behaviors, and help patients cognitively connect a desired action with an existing everyday action.
On the morning of in-person treatment, members receive messages motivating them to come in for their session and to start the day positively. Later in the day, after returning home, members receive additional messaging to encourage them to act on therapeutic principles they learn during their sessions, as well as take other healthy steps in their daily life. Helise said, “When I would get my message every morning, it just reminded me that I was connected to something bigger. It reminded me of the good things here. They talk about being needed and wanted and expected. When I get those messages, I just feel connected to Bridgeway.”
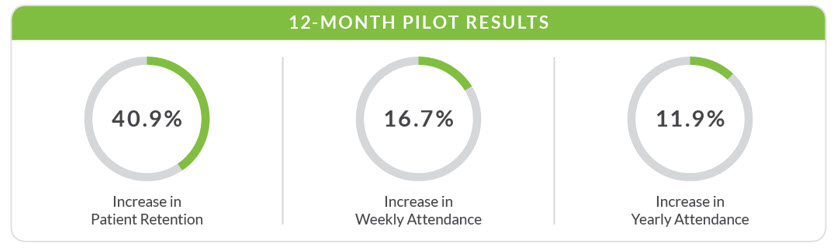
According to Bob Gold, GoMo Health Founder and Chief Behavioral Technologist, “Bridgeway experienced a 17% increase in weekly attendance and an astonishing increase in patient retention from 60% to nearly 90%; both of which resulted in greater annual revenue for the center.”
The Road to Recovery: Recovery Pathways
There is a ripple effect associated with mental health. It can impact other aspects of health and well-being as well as relationships with family and friends. People with mental health conditions are at risk for other medical conditions, including substance use disorders (NAMI-B):
- One in 15 US adults experience both a substance use disorder and mental illness (NAMI-A).
- Nearly one out of three people with mental illness experience substance use disorder (NAMI-A).
Thus, it is vitally important that services exist to address both conditions concurrently. That is the case for the programs offered by the Rimrock Foundation.
Rimrock offers intensive outpatient and residential treatment programs for individuals struggling with addiction, mental health conditions, or court-ordered treatment related to drug felonies. The largest treatment center for adults with substance use and co-occurring disorders in Montana, Rimrock views addiction as a whole person illness, affecting an individual’s emotional, physical, spiritual, and social wellbeing.
In 2020, Rimrock identified an opportunity to improve outcomes by extending care and support outside of the traditional treatment setting. This resulted in the creation and launch of the Recovery Pathways digital health management program in partnership with GoMo Health.
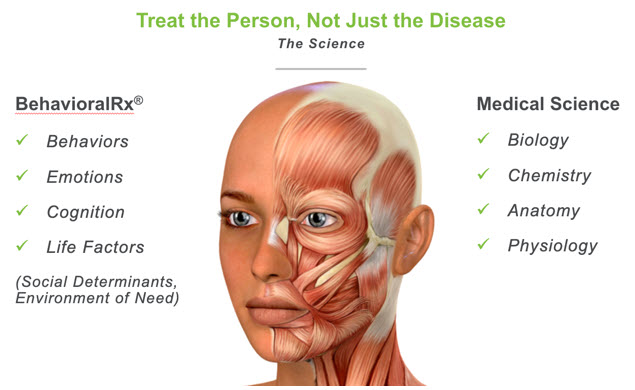
BehavioralRx®, The Science of Precision Health
GoMo Health leveraged its proprietary emerging science, BehavioralRx, to build the program and determine the engagement strategy, approach and content delivered.

Original on-site programming consisted of months of addiction treatment, training, education, and life skills development, individual and group therapy, case management, and peer support. The Recovery Pathways program enhances patients’ experiences by adding text messages delivered several times per week, bolstered with videos and other content designed to reinforce lessons and skills taught in the program and principles covered in therapy. Throughout the program, assessments are delivered to check in on how a patient is doing and escalate to additional care and support available from Rimrock if needed.
The program includes content on preparing patients for required events such as court appearances, maintaining employment, transitioning between phases in the program, promoting self-care, healthy living, behavior change and resiliency, easing re-entry concerns for those who may have served time, and engaging, informing, and supporting caregivers. The program support continues (for six months) even after patients graduate from onsite programs.
The program has been hugely successful, receiving recognition throughout the state as a new gold standard for treating addiction recovery. Achievements include:
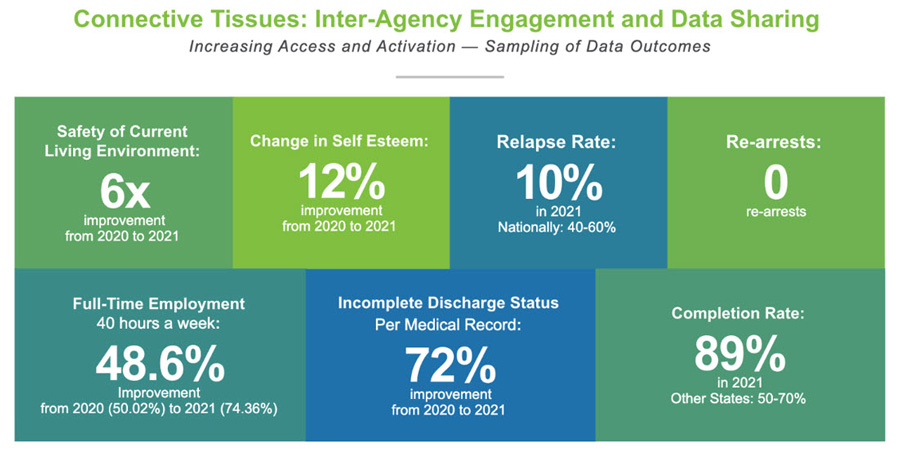
According to Montana Governor, Greg Gianforte, “Recovery Pathways is the result of all three branches of government working together with the best private sector treatment providers and cutting-edge technology to treat addiction as it should be treated, as a disease.”
GoMo Health is advancing the standard of care for mental illness and addiction treatment, leveraging its BehavioralRx® cognitive and behaviorally-based science of patient engagement to provide flexible and adaptive programs that enhance current treatment programs while improving reach, access, and engagement for the populations most at-risk and underserved.
Sue Zbikowski, PhD, is the founder and CEO of inZights Consulting and an Advisory Board Member at GoMo Health. Shelley R. Schoenfeld is Chief Strategist at GoMo Health. For more information about the GoMo Health Behavioral Health Personal Concierge Program and other digital health management programs, please visit https://gomohealth.com/campaigns/dei-in-healthcare/ or text DEI to 43386.
References
Centers for Disease Control and Prevention. [Internet] About Mental Health. What Causes Mental Illness. https://www.cdc.gov/mentalhealth/learn/index.htm. Accessed on 3/3/2023.
National Alliance on Mental Illness (NAMI), California. [Internet] What is Mental illness. Available from https://namica.org/what-is-mental-illness/. Accessed on 3/3/2023.
National Alliance on Mental Illness (NAMI-A). [Internet] Mental Health By The Numbers. Available from https://nami.org/mhstats. Accessed on 3/3/2023.
National Alliance on Mental Illness (NAMI-B). [Internet] Chronic Illness and Mental Health: Recognizing and Treating Depression. NIMH » Chronic Illness and Mental Health: Recognizing and Treating Depression (nih.gov). Accessed on 3/3/2023.
National Institute of Mental Health. [Internet] Mental Illness. Past year prevalence of Any Mental Illness. Available on https://www.nimh.nih.gov/health/statistics/mental-illness. Accessed on 3/3/2023.
Olfson M, Mojtabai R, Sampson NA, Hwang I, Druss B, Wang PS, Wells KB, Pincus HA, Kessler RC. Dropout from outpatient mental health care in the United States. Psychiatry Serv. 2009 Jul;60(7):898-907. doi: 10.1176/ps.2009.60.7.898.
World Health Organization. [Internet] Mental Health. Determinants of Mental Health. https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response. Accessed on 3/3/2023.