Depression and anxiety are among the most prevalent and disabling mental health conditions in the United States. Millions of people face these challenges every year, often with symptoms that interfere with their daily lives. Yet despite the increasing demand for mental health care, many individuals struggle to access timely, effective treatment, particularly those in underserved or rural areas.
Primary care remains the first point of contact for most individuals seeking help, but many clinics lack the infrastructure or specialized staff to provide sustained behavioral health support. Meanwhile, the nationwide shortage of mental health providers continues to limit access, leading to long wait times, inconsistent follow-up, and missed opportunities for early intervention.
The Collaborative Care Model: A Proven Solution
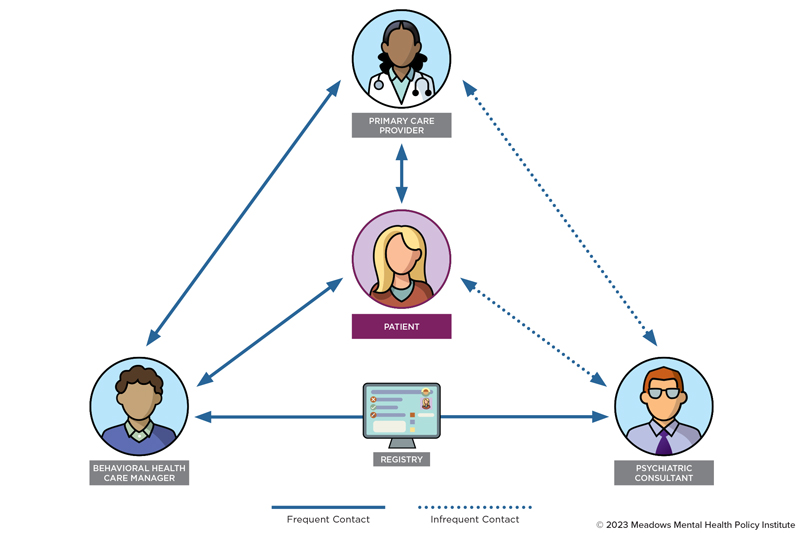
The Collaborative Care Model (CoCM) directly addresses these challenges by embedding behavioral health services within the primary care setting. Developed and extensively studied by researchers at the University of Washington’s AIMS Center, the model is built around a multidisciplinary care team that includes:
- A primary care provider (PCP)
- A behavioral health care manager
- A psychiatric consultant
This team-based approach supports systematic identification and treatment of depression and anxiety using validated tools such as the PHQ-9 for depression and GAD-7 for anxiety. These measures enable measurement-based care, allowing clinicians to track patient symptoms over time and adjust treatment based on real-time clinical outcomes.
How It Works: A Coordinated, Patient-Centered Approach
Collaborative Care offers a fundamentally different experience compared to traditional referral models, which often result in disjointed or delayed treatment. Instead, CoCM emphasizes proactive, coordinated engagement between the care team and the patient.
For example, a patient who visits their PCP with symptoms such as fatigue or sleep disturbances may be screened during the visit. If behavioral health concerns are identified, a behavioral health care manager shortly follows up often by phone or video—to provide support, build rapport, and create a personalized care plan. The psychiatric consultant reviews the case regularly, offering clinical guidance to the care team based on symptom scores and progress.
Regular, structured check-ins help maintain treatment momentum, reinforce coping strategies, and allow for timely treatment adjustments. Importantly, the patient remains connected to their primary care team throughout the process, which builds trust and continuity, especially valuable in communities where stigma or logistical barriers can prevent access to traditional mental health services.
What the Research Shows
Numerous studies have validated the effectiveness of the Collaborative Care Model. A landmark Cochrane review found that CoCM leads to significantly better outcomes for both depression and anxiety compared to usual care, across diverse patient populations and healthcare settings.
More recent real-world data further reinforce the model’s impact. For instance, large-scale implementations have shown that:
- Nearly 50% of patients experience a 50% or greater reduction in symptoms
- Many patients complete treatment in under four months
- Results are consistent across age groups, socioeconomic backgrounds, and care delivery methods, including telehealth
The model has proven especially effective in settings with limited access to specialty care, such as rural clinics, community health centers, and pediatric primary care. Whether delivered in-person or virtually, CoCM has demonstrated its flexibility, scalability, and reliability in supporting mental health recovery.
Looking Ahead: Scalable, Sustainable Mental Health Integration
As health systems search for scalable solutions to the mental health crisis, Collaborative Care stands out as both evidence-based and operationally feasible. It leverages existing primary care infrastructure, strengthens care coordination, and delivers results that matter to patients and providers alike.
By embedding behavioral health into the everyday delivery of care, CoCM offers a path forward—one that meets patients where they are, supports them through recovery, and ultimately changes the way mental health is treated across the healthcare system.
Virna Little, PsyD, LCSW-r, MBA, CCM, SAP, is the Co-founder and Jian Joyner, LSW, is a Research Assistant at Concert Health. For questions about this article, please contact Dr. Virna Little, a national expert and advocate in Collaborative Care, at virna@concerthealth.io.
References
Archer, J., Bower, P., Gilbody, S., Lovell, K., Richards, D., Gask, L., Dickens, C., & Coventry, P. (2012). Collaborative care for depression and anxiety problems. The Cochrane Database of Systematic Reviews, 10(10), CD006525. https://doi.org/10.1002/14651858.CD006525.pub2
Caspi, A., Houts, R. M., Moffitt, T. E., Richmond-Rakerd, L. S., Hanna, M. R., Sunde, H. F., & Torvik, F. A. (2024). A nationwide analysis of 350 million patient encounters reveals a high volume of mental-health conditions in primary care. Nature Mental Health, 2(10), 1208–1216. https://doi.org/10.1038/s44220-024-00310-5
Counts, N. (2023, May 18). Understanding the U.S. behavioral health workforce shortage. The Commonwealth Fund. https://www.commonwealthfund.org/publications/explainer/2023/may/understanding-us-behavioral-health-workforce-shortage
Hardy, C., Green, B., Little, V., & Vanderwood, K. (2024). Clinical variables associated with successful treatment of depression or anxiety in collaborative care. Journal of Behavioral Health Services & Research, 51(4), 599-608. https://doi.org/10.1007/s11414-024-09892-5
Modi, H., Orgera, K., & Grover, A. (2022). Exploring barriers to mental health care in the U.S. Washington, DC: AAMC. https://doi.org/10.15766/rai_a3ewcf9p
Vanderwood, K., Joyner, J., & Little, V. (2023). The effectiveness of collaborative care delivered via telehealth in a pediatric primary care population. Frontiers in Psychiatry, 14, 1240902. https://doi.org/10.3389/fpsyt.2023.1240902
Walker, C., Little, V., Joyner, J., Fuller, S., & Green, B. (2024). Factors influencing virtual collaborative care outcomes for depression and anxiety. Journal of Family Medicine and Primary Care, 13(5), 1968-1974. https://doi.org/10.4103/jfmpc.jfmpc_1493_23