The year was 2014, and Drexel University, where I was working at the time, partnered with Pennsylvania’s Office of Mental Health and Substance Abuse Services (OMHSAS) in submitting and being awarded a 5-year, $736,000 annually Garrett Lee Smith (GLS) grant for youth suicide prevention.
Our main goals were to:
- Increase the number of:
- staff in schools, colleges, and universities trained to identify/refer youth at risk for suicide
- youth screened and referred for treatment
- clinical service providers trained to assess, manage, and treat youth at risk for suicide
- Increase awareness about youth suicide prevention among youth, families, educators, and community members
- Promote statewide, systems-level change to advance suicide prevention efforts
Ten years and another 2019-2024 $3.68 million PA GLS grant later, we are reviewing our accomplishments and where we need to head next.
2014-2019 PA GLS Grant Program
The “Suicide Prevention in Pennsylvania Schools and Colleges Initiative” from 2014-2019 implemented suicide prevention and early intervention strategies for youth ages 10 to 24 across the commonwealth. During those years, we screened 13,000 Pennsylvania students and identified 4,300 youth with some level of suicidal ideation. We did this using a software platform that allowed us to obtain electronic consent, identify and screen students, and gather real-time data to identify resource needs over time. It had the ability to connect the Student Assistance Program (SAP) agencies across the state using the software for data collection and outcome measures. The software accomplished our “systems-level” change and provided a new statewide infrastructure.
Initially developed through a collaboration with the Children’s Hospital of Philadelphia (CHOP), the software, with its Behavioral Health Screen (BHS), has been validated and researched by clinicians and experts in the fields of psychiatry, psychology, and pediatrics. Over the last 20 years, a validation process generated a stream of scientific knowledge which can guide clinical practice, and study findings have found connections between sexual identity and disordered eating, adolescent risk factors for suicide ideation, and links between depression, substance use, and non-suicidal self-harming behavior.
When it comes to technology, additions, improvements, and innovation are constant. The software platform evolved, and our SAP agencies benefited each year from enhanced referral management for documenting attended services, a BHS child version, SAP assessment file; interactive dashboards for screening and assessment data; the launch of a case notes module, a telehealth module, and an indirect services module; and a BHS Spanish version.
Using this software technology increased the identification of youth at risk for suicide in the targeted population from 8% to 33% and has offered us a way to measure behavioral health across demographics, regions, and shared risk factors.
2019-2024 PA GLS Grant Program
The 2019 – 2024 Pennsylvania GLS program involved collaborations between investigators at Thomas Jefferson University and Drexel University, as well as partnerships with county and local leaders from several target counties around Pennsylvania. We called it “Pennsylvania Resource for Continuity of Care in Youth-Serving Systems and Transitions (PRCCYSST) – “PERSIST.”
Using a two-tiered model, this project targeted youth ages 10-24. Tier 1 was statewide and provides awareness, training, and screening activities to equip mental health professionals and the general public to increase identification and improve outcomes for youth at risk. Tier 2 worked with target counties to promote systemic change to improve continuity of care between youth-serving systems for those at risk of suicide. Again, we relied on the same technology infrastructure to continue our progress.
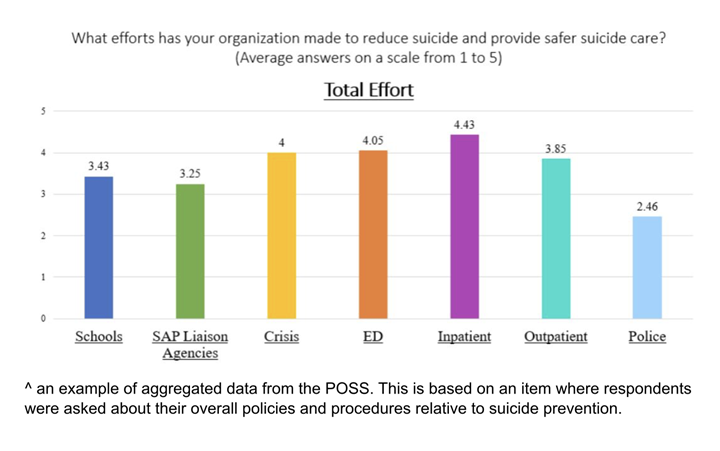
The program focused on an extensive data collection process whereby representatives from youth-serving systems completed the Pennsylvania Organizational Self-Study (POSS), a needs assessment adapted for each system to fit their anticipated needs and best-practice goals. The results of this assessment were aggregated by county and presented back to county and system leaders so that they might see where their strengths and needs exist.
Additionally, a smaller cohort of some of the same agencies participated in the Pennsylvania Network Analysis (PANA), which utilized cutting-edge network science to highlight connections, both unidirectional and bidirectional, between youth-serving systems in a given county. Results from the PANA allowed counties to see in a map-like format how data and information are shared both within agencies of the same system type as well as across systems, visualizing where strong continuity of care exists in a county and where the opportunity remained to grow it.
Activities from this PA GLS grant term also included statewide efforts aimed at increasing awareness for suicide prevention, such as the continuation of the Higher Education Suicide Prevention Coalition (HESPC), new courses added to the Prevent Suicide PA Online Learning Center, and the annual Prevent Suicide PA Youth PSA Contest for Suicide Prevention, where high school students across the Commonwealth created and submitted poster, video, and audio entries showcasing their creative talents and engage their peers in suicide prevention.
The Behavioral Health Learning Collaborative (BHLC) of Pennsylvania continues to bring together SAP agencies in more than 70% of the state’s counties to provide updates on the software platform and invite agencies to share their latest achievements and lessons they have learned in identifying and supporting students at risk of suicide. This network has generated best practices and high-quality research that can benefit both state and local programs throughout the country. We created a web-based hub to share this information with the public and to continue our collaborative efforts outside of funding cycles.
The Future of Behavioral Health Technology
As we plan for 2025 and beyond, we will continue using this software technology to achieve our goal of preventing as many youth suicides at the highest rates possible. This includes the integration of artificial intelligence – which enables computers to perform a variety of advanced tasks – to aid us. We know a comprehensive student mental health system connected with technology identifies conditions early, and early detection and treatment saves lives.
Tita Atte, MPH, CPH, is the Director of Screening and Program Evaluation and Director of CQI Data Analytics at the David Farber ASPIRE Center, Thomas Jefferson University, Vickie and Jack Farber Institute for Neuroscience, Department of Psychiatry & Human Behavior. For more information, email: tita.atte@jefferson.edu.
Author’s Note: The two grants were funded under awards SM061750 and SM082107 by the Substance Abuse and Mental Health Services Administration (SAMHSA). The views expressed herein do not necessarily reflect the official policies of the U.S. Department of Health and Human Services, nor does mention of trade names, commercial practices, or organizations imply endorsement by the U.S. Government.
The views and content of this article do not necessarily reflect the official policies or views of the Commonwealth of Pennsylvania, specifically the Office of Mental Health and Substance Abuse Services, the Department of Drug and Alcohol Programs, and the Department of Education, nor does mention of trade names, commercial practices, or organizations imply endorsement by these entities.






