An implantable device detected opioid overdose and automatically administered naloxone, saving lives in rat and pig models.
The device hasn’t yet been tested in people. If successful, it might also be adapted to treat other emergencies, such as life-threatening allergic reactions.
Almost 75,000 people in the U.S. die every year from an overdose involving opioids. Opioids include prescription medications, such as oxycodone and hydrocodone, as well as illegal drugs like heroin and fentanyl.
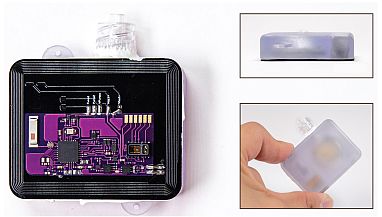
The Naloximeter device for large animals. At 42 mm (1.65
inches) by 34 mm (1.34 inches) by 13 mm (0.5 inches), it is
about three-quarters the size of a commercial pacemaker.
Credit: Ciatti et al., Science Advances
During an opioid overdose, breathing slows dangerously. This prevents enough oxygen from reaching the brain and other vital organs. If the overdose isn’t reversed within minutes, it can result in brain damage or death.
A medication called naloxone, also known as Narcan, can almost instantly reverse an opioid overdose. It attaches to opioid receptors on cells and blocks opioid drugs. Laws have expanded access to naloxone over the last several years. But it needs to be given immediately, and by another person. Overdoses often occur when someone is alone.
To overcome these limitations, a research team led by Dr. Robert Gereau IV from Washington University School of Medicine in St. Louis and Dr. John Rogers from Northwestern University has been developing a device to automatically detect an opioid overdose and deliver naloxone.
Their device, which they call the Naloximeter, is about three-quarters the size of a pacemaker and can be implanted under the skin. A sensor in the battery-powered device detects when oxygen levels start to drop. It then sends a warning signal to a nearby phone or tablet. If the warning isn’t overridden, the device releases a dose of naloxone. It can also broadcast an emergency alert to first responders.
In their new study, funded in part by NIH, the team tested versions of the device in rats and pigs. Results were published on October 25, 2024, in Science Advances.

Implanted under the skin, the Naloximeter senses dropping
oxygen in the surrounding tissues and sends a warning
notification to a mobile application. If the user doesn’t engage
with the warning message within 30 seconds, it releases
naloxone and can send an alert to first responders.
Credit: Eric Young
A miniature version of the device using wireless powering instead of a battery was first tested in rats. After administration of fentanyl, the device detected overdose within a minute and released naloxone. Treated rats showed full recovery from overdose within five minutes.
The researchers next tested a battery-powered device in pigs, which are more similar to people. They tested two different methods for the device to deliver naloxone: through a tiny catheter directly into a vein or into surrounding tissue using a small injection needle.
In pigs, the Naloximeter detected fentanyl overdose in less than two minutes. When the device released naloxone directly into the bloodstream, pigs recovered within 10 minutes of overdose. The device with a needle required backup manual administration because needle delivery did not get naloxone into the bloodstream from the surrounding tissue fast enough.
The team is performing additional research to improve the performance of the injection version, which may be safer for long-term implantation. They’re also addressing additional challenges for eventual use in people, including battery life. If proven to be effective in people, the Naloximeter could be an important tool to help save lives amid the overdose crisis.
The device may also have potential applications beyond reversing overdose. “The Naloximeter is a proof-of-concept platform that isn’t limited to the opioid crisis,” says Joanna Ciatti, a graduate student in Rogers’ lab who worked on the study. “This technology has far-reaching implications for those threatened by other emergent medical conditions such as anaphylaxis or epilepsy.”
References
An autonomous implantable device for the prevention of death from opioid overdose. Ciatti JL, Vázquez-Guardado A, Brings VE, Park J, Ruyle B, Ober RA, McLuckie AJ, Talcott MR, Carter EA, Burrell AR, Sponenburg RA, Trueb J, Gupta P, Kim J, Avila R, Seong M, Slivicki RA, Kaplan MA, Villalpando-Hernandez B, Massaly N, Montana MC, Pet M, Huang Y, Morón JA, Gereau RW 4th, Rogers JA. Sci Adv. 2024 Oct 25;10(43):eadr3567. doi: 10.1126/sciadv.adr3567. Epub 2024 Oct 23. PMID: 39441938.
This article was originally published on November 5th, 2024, and can be found here.



