As the United States grapples with the realities of an aging population, the importance of adapting our health and social service system of care to meet the needs of older adults has never been more critical. In 2020, approximately one in six people in the U.S. were aged 65 or over, highlighting a significant demographic shift. This group has now reached 55.8 million or 17% of the total population, which is a 38.6% increase over the previous decade.
The older population not only requires more healthcare resources but also needs tailored behavioral health services that are sensitive to the complexities of aging. America’s Health Rankings Senior Report points out a number of health disparities among older adults that impact overall healthcare and calls out the required changes needed in the healthcare system in order to innovate and expand services that cater specifically to this age group.
A recent SAMHSA report [2021 and 2022 National Surveys on Drug Use and Health (NSDUH)] provides critical insights into the behavioral health trends among older adults, focusing on substance use, mental health, and treatment needs within this demographic.
Listed below are a few of the relevant findings from this report:
- An estimated 12.5% of older adults had any mental illness (AMI) in the past year, with a smaller subset (1.9%) experiencing serious mental illness (SMI).
- About 16% of older adults received some form of mental health treatment in the past year, but there is a large perceived unmet need for mental health services among those who recognize their issues but do not seek help.
- Around 9% of older adults had a substance use disorder in the past year, but fewer than one-third of those who needed substance use treatment actually received it.
- Perceptions regarding the need for treatment were also skewed, with a significant majority of those needing treatment not recognizing the need.
- Approximately 12% of older adults reported using illicit drugs in the past year, with older adult males more likely than females to use these substances.
Additionally, other studies [1][2] consistently show very low rates of mental health treatment utilization among older adults, with the majority (60-70%) not receiving services despite having clinically diagnosed mood, anxiety, or substance use disorders.
In order to address these findings and the disparities in access to needed services, supports, and treatments, there are a number of recommendations in the report that must be systematically implemented. All of these underscore the importance of developing targeted strategies to support the mental health and substance use challenges faced by an older population, emphasizing the need for policy adjustments, specifically tailored interventions, and more strategically focused resource allocation to meet these growing needs.
Best-Practices
Enhanced Screening and Access: We must improve routine screening, especially during primary care visits, for substance use and mental health disorders among older adults, using validated tools like the Alcohol Use Disorders Identification Test (AUDIT) and Geriatric Depression Scale. [3][4] Integrating screening into primary care settings, where older adults more frequently access services, can help identify those in need of intervention and referral to specialized treatment.[5] Enhanced screening must be paired with better access to treatment services, such as integrated care or collaborative care model, where there are significantly higher treatment engagement rates compared to referrals to separate clinics (71% vs 49% engagement).[6]
Addressing Gender Differences: We must develop and implement tailored interventions to address the distinct needs of older men and women, particularly as it relates to substance use and mental health treatment and services. SAMHSA’s Treating Substance Use Disorder in Older Adults highlights several such programs, including:
- Women’s Integrated Treatment (WIT) is a group-based intervention that integrates psychoeducational and cognitive-behavioral techniques to address substance misuse, trauma, and mental health issues common among older women.
- Men’s Integrated Substance Abuse and Trauma Treatment (MINSATT) is a group therapy program tailored for older male veterans with PTSD and substance use disorders.
Integration of Services: Coordinated care approaches that integrate physical health, mental health, and substance use treatments have shown promising results in improving outcomes for older adults. One of the most successful integrated care approaches is the Collaborative Care Model, which involves multi-disciplinary teams – including primary care providers, care managers, and behavioral health specialists – working together to manage patients’ care. Studies show that this model not only improves the quality of care but also enhances patient satisfaction and reduces healthcare costs by focusing on holistic treatment rather than separate treatment streams for mental and physical health.
Innovative care coordination and navigator programs have also been proven effective. For example, the Wellness Recovery Teams program involves navigators, registered nurses, and behavioral health professionals who work together to provide comprehensive care for adults with serious mental illness (SMI) who also have chronic medical conditions. This program has been linked to a reduction in emergency department visits and inpatient admissions while also improving patients’ engagement with primary care and specialist services.
Public Awareness and Education: Increasing awareness about the signs of substance misuse and mental health disorders in older adults can help in reducing stigma and increasing early identification and intervention. Initiatives like Screening, Brief Intervention, and Referral to Treatment (SBIRT) train primary care providers to screen, provide brief interventions, and refer to treatment as needed. Raising public and provider awareness through campaigns, training healthcare professionals, integrating screening into routine care, and developing specialized programs for older adults can improve early identification and access to appropriate treatment services for this underserved population.
Technology-Assisted Care Solutions
Today, technology is an integral part of our daily lives, regardless of age, gender, or socioeconomic background, and the healthcare sector has embraced technology-assisted care solutions as important tools in improving outcomes. According to the 2024 Behavioral Health Industry Trends Report, many behavioral health organizations still lag in innovating with technology, but there’s a growing push to integrate technology-assisted care solutions to improve service delivery and outcomes.
The integration of new technology-assisted care solutions into geriatric healthcare represents a paradigm shift in how geriatric care will be delivered, potentially making it more proactive, personalized, and accessible. The use of advanced technologies such as telemedicine, artificial intelligence (AI), and wearable devices can not only improve access to healthcare but also facilitate treatments and interventions that are tailored to the individual needs of older adults. As technology continues to evolve, the focus must remain on personalizing care to meet the complex health needs of older adults with precision and compassion, ensuring better health outcomes and improved quality of life.
Emerging best practices in the use of technology-assisted care solutions in geriatric care should include the development of comprehensive care models that combine telehealth, AI, and wearable technologies to provide more holistic care solutions.
- Telehealth: Multiple studies have shown the transformation in healthcare delivery through telehealth, most notably during the COVID-19 pandemic. The utilization of telehealth has continued to surge, proving particularly valuable in geriatric care. Telehealth platforms facilitate real-time video consultations, which are critical not only for routine health assessments but also for mental health evaluations where the physical presence of a healthcare provider may not be necessary. These virtual visits have been shown to reduce the stigma or reluctance associated with visiting mental health settings, a significant barrier among older adults. These technologies offer enhanced accessibility, efficiency, and responsiveness to patient needs. For geriatric care, telehealth has been vital in providing continued access to healthcare services for older adults, particularly in remote and underserved areas.
- Advanced Analytics and Personalized Care: Leveraging big data and advanced analytics, healthcare providers have the potential to offer more personalized care to older adults. By analyzing vast amounts of health data, including prior medical history and even real-time data from wearable devices, AI will eventually be able to better predict health deterioration and assist the provider in adjusting medications and customizing treatment plans to meet the individual’s unique needs.
- Artificial intelligence (AI): The use of AI is growing in diagnosing and managing cognitive health issues prevalent among older adults, such as dementia and Alzheimer’s disease. AI algorithms can analyze speech patterns and physical movements to detect early signs of cognitive decline. Many companies are pioneering AI projects that can sort through complex clinical data to assist in developing personalized treatment plans that adjust to the cognitive abilities of the patient.
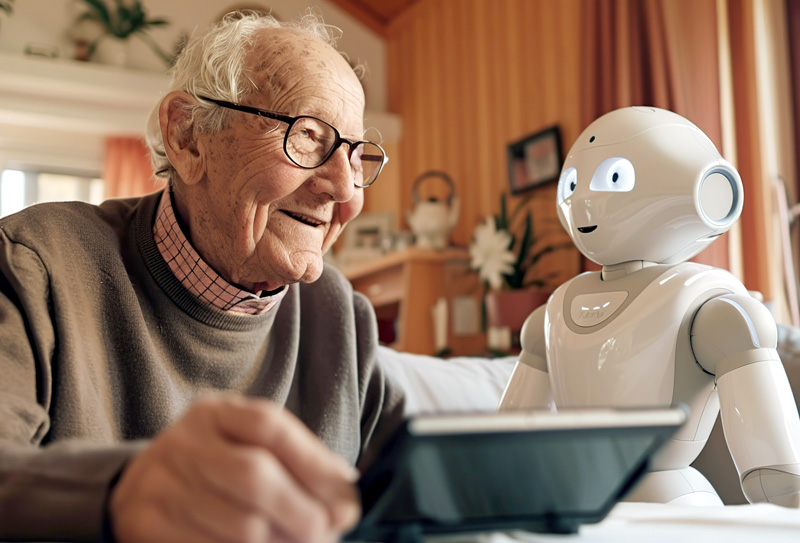
- Robotics in Elder Care: Robotic technology, while still not mainstream yet, is finding its way into geriatric care, providing physical assistance and companionship to older adults. Robots like Mabu and PARO can help manage daily activities and improve mental health by reducing feelings of loneliness and social isolation.
- Wearable Technology: These are increasingly being used to monitor the health of older adults. Devices equipped with sensors can track vital signs, detect falls, and monitor physical activity levels, providing real-time data to healthcare providers. The use of such technology, currently being supported by the National Institute on Aging, can assist in managing chronic conditions and preventing emergencies by allowing timely medical interventions.
While the integration of technology-assisted care solutions in geriatric care offers certain benefits, especially in managing certain mental health and substance use challenges, the vetting, purchasing, implementation, integration, and monitoring of these technologies is not without its obstacles. If these obstacles are not systematically considered and addressed from inception, the implementation and ultimate effectiveness of these technology-assisted care solutions in geriatric care may be hindered.
A major hurdle is the digital divide that affects many older adults, characterized by limited access to the internet and the necessary devices. This gap is more pronounced in rural and underserved areas where broadband infrastructure is often inadequate. Additionally, the high cost of implementing cutting-edge technologies can be prohibitive for many healthcare organizations or facilities, particularly those operating under tight budget constraints or serving economically disadvantaged populations. Beyond the costs, there are issues of data security, data sharing, and system(s) integration and interoperability that are critical to consider.
Another significant challenge is the need for comprehensive training for healthcare providers. The effective use of advanced technologies requires not only initial training but also ongoing education to keep up with evolving tools and applications. This training must be tailored to include practical skills in operating the technology and understanding how to integrate digital solutions into existing care protocols effectively.
The reality is that patients and healthcare providers may have reservations about the shift from traditional face-to-face interactions to digital platforms. For many older adults, personal interaction is a crucial element of trust and comfort in their healthcare experience. Overcoming skepticism and building confidence in using these technology-assisted solutions is essential, requiring ongoing efforts to demonstrate the safety, efficacy, and personal benefits of these tools.
Addressing these challenges will require a multi-faceted approach. Infrastructure improvements, particularly in rural and underserved areas, are crucial for ensuring access to telehealth and other digital health services. Funding initiatives, possibly through public-private partnerships or state and federal grants, could alleviate the financial pressures associated with technology adoption. Educational programs designed to enhance digital literacy among older adults and training for healthcare providers can help mitigate some of the cultural and operational barriers. Encouraging the development of user-friendly technology that considers the unique needs of older adults – such as simplified interfaces and enhanced accessibility features – will go a long way to increase acceptance and usage.
What is needed is an organized effort to address the policy, programmatic, structural, technical, financial, and cultural barriers to implementing these tailored best practices in geriatric care, and we must start paving the way for more widespread adoption of these emerging technology-assisted care solutions in our healthcare system…with the goal of ultimately leading to better health outcomes for older adults.
Jorge R. Petit, MD, is a Behavioral Healthcare Leader, Author, and Founder/CEO of Quality Healthcare Solutions, LLC. Dr. Petit is also a long-time Board Member and past Chair of Mental Health News Education, the publisher of Autism Spectrum News and Behavioral Health News. For more information, visit his website: www.drjpetit.org, blog: Behavioral Health: Matters, LinkedIn: Dr. Jorge Petit, MD, or Substack: drjrpetit.substack.com.




