Our healthcare and social welfare systems face grave challenges amid an unprecedented demand for services. The acute economic instability of recent years, environmental degradation attributable to global climate change, and chronic sociopolitical upheaval have compromised public health and wellbeing on a scale unimaginable merely a generation ago. “Existential angst” associated with these trends has become the predominant psychological state for many. For some, this is manifest as a subclinical emotional malaise. For others, it emerges as severe anxiety, dysphoria, and similarly debilitating conditions. Unparalleled rates of suicide and substance misuse and abuse have followed. An outsized demand for services driven by the foregoing factors occurs at a time when our systems are ill-equipped to deliver on their missions. This is a consequence of several factors, foremost of which is an enduring workforce crisis that has produced a dire shortage of qualified providers throughout the country. Moreover, providers must fulfill increasingly onerous administrative demands and have little time to attend to their clients’ needs. Nothing short of transformative solutions is required to correct this structural dysfunction and to restore our systems’ capacity to “meet the moment.” Potential solutions may be found in Artificial Intelligence (AI) and other digital technologies if they are deployed appropriately. To paraphrase Albert Einstein, AI might constitute an opportunity embedded in a crisis.

AI encompasses a diverse array of technological applications that mimic human cognitive functions such as learning and problem-solving. It has yielded certain benefits in various facets of the service delivery process and exceeded the performance of human experts in some instances. It has been widely deployed within the realm of medical imaging, in which it has been proven to analyze diagnostic images with greater precision than radiologists when applied to select specialties, including radiology, dermatology, and pathology (Bajwa et al., 2021). It has also been shown to aid clinicians in clinical decision-making, specifically in the realms of disease classification (i.e., diagnosis) and prognosis (Khosravi et al., 2024).
The use of AI in the behavioral healthcare (BH) and social service sectors has been more limited, however. These sectors often face acute resource limitations that preclude the deployment of new technologies, many of which are prohibitively expensive, particularly if accessed during their incipient phase of development (Glauser, 2024). AI’s application to BH is also limited by factors unique to this specialty. Diagnostic measures utilized within medical and surgical specialties such as diagnostic imaging, blood tests, and urinalysis, among countless others, entail substantial quantitative components that may be readily accessed and analyzed by emerging digital technologies. By contrast, BH relies primarily on providers’ capacity to assimilate qualitative information from disparate sources and to render judgements that reflect both the information received and innumerable contextual factors that inform the interpretive process. These limitations notwithstanding, AI may aid BH providers in aggregating and summarizing clinical documentation essential to the assessment process. It has also proven effective in the realm of “digital phenotyping,” an emerging technology that entails the use of digital information to evaluate individuals’ emotional and psychological states through analyses of content shared on social media platforms, email and text communications, and other sources. These analyses may reveal changes in behavior indicative of certain risk factors. AI has also aided BH providers through remote sensing and ambient applications designed to monitor aspects of recipients’ physiology or environmental conditions relevant to their emotional and psychological wellbeing. For instance, commercially available technologies such as Google Nest are now equipped to monitor users’ sleep patterns using motion and sound sensors, and data obtained may reveal anomalies associated with certain behavioral health conditions (Muoio, 2021).
AI may also reduce BH providers’ administrative workload when used to simplify or streamline service documentation processes. This is a realm of untapped potential, particularly for social welfare providers who depend heavily on paraprofessionals who operate at the confluence of several trends that have exacerbated the strain on their profession and perpetuated a workforce crisis. Social welfare organizations commonly serve individuals with exceptionally complex needs within intricate fiscal and regulatory environments. Their employees must deliver services, fulfill increasingly onerous documentation requirements, and meet innumerable other demands in exchange for modest compensation. Although much of the research concerning the use of AI in alleviating providers’ documentation burden explores its application within “traditional” healthcare settings (e.g., primary care clinics, hospitals, etc.), some findings may be extrapolated to other settings. One study that investigated the use of ambient AI “scribes” among physicians affiliated with The Permanente Medical Group (TPMG) found this technology reduced the amount of time study participants spent preparing documentation, thereby increasing the time available for service delivery and patient engagement (Tierney et al., 2024). Another study explored the impact of a similar technology utilized among family medicine practitioners and revealed similarly salutary results. Practitioners who adopted this technology reported a 72% median reduction in documentation time, statistically significant improvements in overall work satisfaction, and fewer signs of professional burnout (American Academy of Family Physicians, 2021). Other studies described beneficial applications of “voice-to-text” technologies that employ recent advances in Natural Language Processing (NLP) to accelerate the documentation process and AI-enabled document summarization tools that aid providers in gleaning essential details embedded in lengthy text documents.
The “use cases” described above are not exhaustive, nor do they constitute panaceas for the behavioral health and social welfare sectors, whose challenges are significant and multifaceted. Nevertheless, as providers optimize their operations via the pursuit of the “Quadruple Aim” – a laudable goal that, if achieved, enhances the patient experience, improves population health, reduces the cost of care, and promotes employee satisfaction and wellbeing – the judicious application of AI may yield substantial benefits that cannot be realized through conventional (i.e., human) means alone.
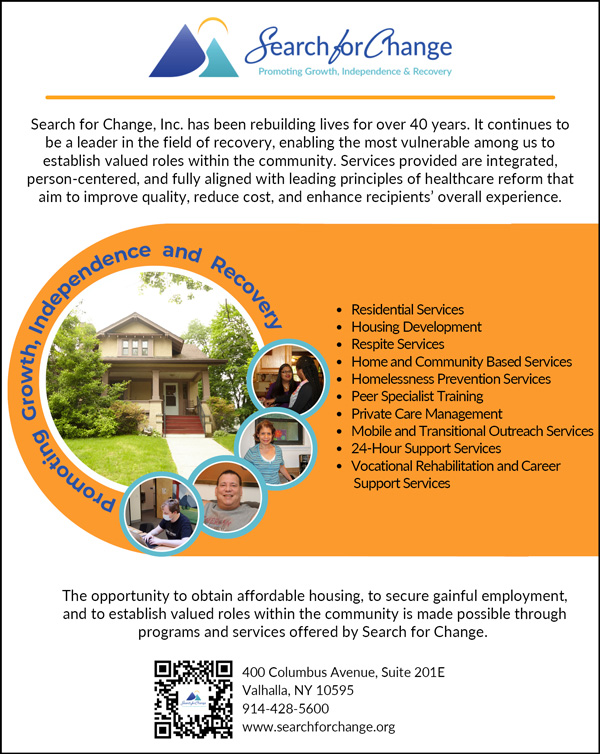
Ashley Brody, MPA, CPRP, is Chief Executive Officer at Search for Change, Inc. He may be reached at (914) 428-5600 (x9228) or abrody@searchforchange.org.
References
American Academy of Family Physicians. (2021). Using an AI assistant to reduce documentation burden in family medicine. https://www.aafp.org/dam/AAFP/documents/practice_management/innovation_lab/report-suki-assistant-documentation-burden.pdf
Bajwa, J., Munir, U., Nori, A., & Williams, B. (2021). Artificial intelligence in healthcare: Transforming the practice of medicine. Royal College of Physicians, 8(2), 188-194. https://doi.org/10.7861/fhj.2021-0095
Glauser, S. (2024, February 9). Why IT is so expensive & what you can do about it. Blue Tree Technology Group. https://bluetreetg.com/why-it-is-so-expensive-what-you-can-do-about-it/
Khosravi, M., Zare, Z., Mojtabaeian, S.M., & Izadi, R. (2024). Artificial intelligence and decision-making in healthcare: A thematic analysis of a systematic review of reviews. Health Services Research and Managerial Epidemiology, 11, 1-15. https://doi.org/10.1177/23333928241234863
Muoio, D. (2021). Google’s next-gen Nest Hub debuts with contactless sleep monitoring and analysis features. Mobi Health News. https://www.mobihealthsnews.com/news/googles-next-gen-nest-hub-debuts-contactless-sleep-monitoring-and-analysis-features
Tierney, A.A., Gayre, G., Hoberman, B., Mattern, B., Ballesca, M., Kipnis, P., Liu, V., & Lee, K. (2024). Ambient artificial intelligence scribes to alleviate the burden of clinical documentation. New England Journal of Medicine, 5(3), 1-15. https://doi.org/10.1056/CAT.23.0404