Substance Use Disorders (SUDs) present a complex and multifaceted public health challenge that disproportionately affects marginalized communities, exacerbating existing health disparities and social inequities. These marginalized populations encompass groups facing social, economic, and structural disadvantages, including racial and ethnic minorities, individuals of lower socioeconomic status, LGBTQ+ individuals, and those experiencing homelessness or justice involvement. The impact of SUD within these communities extends beyond individual health concerns, encompassing broader social, economic, and systemic implications. Enhancing access to addiction services and reducing barriers within a social justice and health equity framework demands a multifaceted approach that intentionally addresses systemic, structural, and individual factors.

Jorge R. Petit, MD
Racial and ethnic disparities in prevalence rates of substance use disorders (SUDs), as well as overdose deaths, are compounded by many factors, such as, historical trauma, systemic racism, limited access to quality healthcare/insurance, accessibility of treatment services, chronic stressors, lack of access to education and employment opportunities, and childcare/transportation barriers, to name a few.
Research consistently reveals that racial and ethnic minority groups, such as African Americans, Hispanics, and Indigenous peoples, often exhibit higher rates of SUD compared to White populations. Homelessness is linked to a higher addiction and SUD risk; many homeless individuals also struggle with mental health issues, unemployment, food insecurity, and limited healthcare access. LGBTQ+ individuals face unique stressors like discrimination, family rejection, and isolation, leading to higher substance use rates as a coping mechanism. Incarcerated individuals are more likely to have a history of addiction and SUD. Marginalized youth, like those in foster care or involved with child welfare systems, have elevated SUD rates. Adverse childhood experiences, trauma, and disrupted family structures contribute to their susceptibility to substance misuse.
Recent data from the Key Substance Use and Mental Health Indicators in the United States: Results from the 2021 National Survey on Drug Use and Health indicated that the percentage of people aged 12 or older who used illicit drugs in the past year was higher among American Indian or Alaska Native (36%) or Multiracial individuals (35%) than among Black (24%), White (23%), Hispanic (19%), or Asian individuals (11%) (see Figure 1 below).
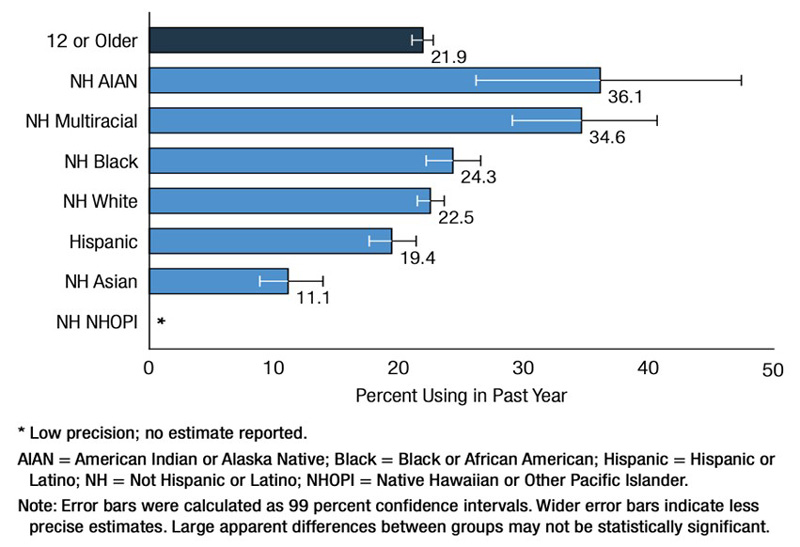
Figure 1: Past Year Illicit Drug Use: Among People Aged 12 or Older; by Race/Ethnicity, 2021
Similarly, the 2020 CDC Vital Signs Report revealed that overdose death rates (number of drug overdose deaths per 100,000 people) increased 44% for Black individuals and 39% for American Indian and Alaska Native (AI/AN) individuals compared to 2019 (see Figure 2 below). Overdose death rates in older Black men were nearly 7x as high as those for older White men and in counties with greater income inequality, overdose deaths for blacks were 2x as high compared to communities with less income inequality.
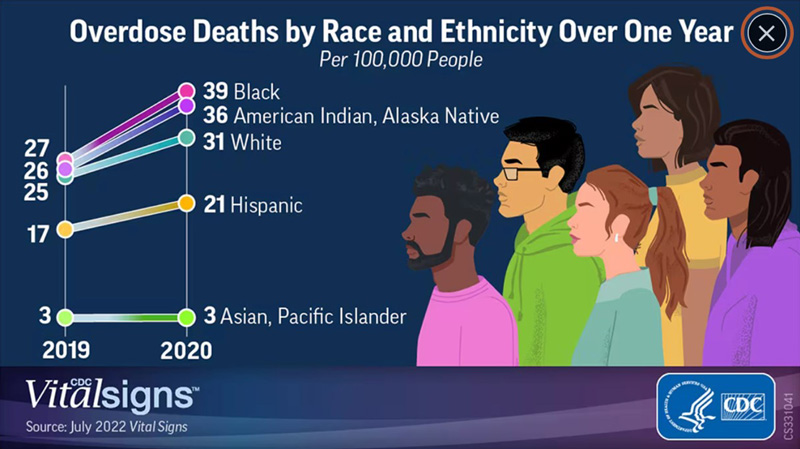
Figure 2: Overdose Deaths by Race and Ethnicity Over One Year
Furthermore, SUD can exacerbate other existing health disparities; individuals grappling with SUD often experience poorer physical and mental health outcomes, including an increased risk of infectious diseases, mental health disorders, and chronic illnesses. The co-occurrence of SUD and other health conditions further strains the healthcare system’s capacities and leads to inferior overall health outcomes.
Numerous barriers exist when seeking SUD treatment, including limited access to healthcare facilities, transportation challenges, lack of insurance coverage, and cultural stigma associated with seeking help for addiction. These barriers impede timely and effective interventions, resulting in delayed or inadequate care. In a 2020 study, Black patients were half as likely to obtain treatment following non-fatal overdose compared to Hispanics and Whites. The economic burden of addiction, encompassing healthcare costs, lost productivity, legal involvement, and strain on social services, can perpetuate cycles of poverty and hinder economic mobility.
Language barriers and cultural insensitivity in healthcare settings can alienate marginalized individuals seeking SUD services. Cultural factors may influence how addiction is perceived, acknowledged, and addressed within different communities, necessitating culturally competent care to ensure effective treatment.
The impact of SUD on marginalized communities intersects with various social determinants of health, such as housing instability, food insecurity, and lack of access to education and employment. These create a cycle of disadvantage that not only contributes to the onset of SUD but also obstructs recovery and sustained wellness. SUD can perpetuate across generations within marginalized communities, establishing a vulnerability cycle. Children born to parents with SUD may experience adverse childhood experiences, heightening their likelihood of developing SUD themselves. This cycle underscores the necessity of comprehensive prevention and intervention efforts.
The impact of SUD extends beyond individuals to entire communities. Elevated addiction and SUD rates can strain community resources, disrupt family structures, and contribute to an environment of instability and insecurity. Recovery necessitates a support network, access to treatment programs, and resources to navigate challenges. Marginalized individuals often lack these essential resources, hindering their ability to overcome addiction successfully and attain sustained recovery.
In my estimation, the principles of Social Justice must be grounded in the pursuit of fairness, equality, and the elimination of systemic health disparities. These principles are highly relevant to SUD prevention and treatment, offering a framework for equitable care access, disparities resolution, and ensuring that all individuals receive the supports and treatment necessary for their recovery.
Efforts to address SUD in marginalized populations must consider the underlying social determinants of health, provide culturally sensitive, inclusive, and trauma-informed care, and offer accessible treatment while reducing stigma, focusing on community-based interventions. Tailored prevention and treatment strategies for these populations can contribute to reducing systemic health disparities.
Addressing the significance of SUD within marginalized communities demands a comprehensive approach that incorporates health equity initiatives, targeted policies, culturally sensitive interventions, and acknowledges the unique challenges faced by these communities. Providing tailored solutions is crucial to reducing SUD-related health disparities, breaking cycles of disadvantage, and fostering a more equitable and just society. Such efforts can enhance individual well-being and strengthen the resilience of entire communities.
Resources
988 Suicide & Crisis Lifeline: 988 Lifeline provides 24/7, free and confidential support for people in distress, prevention and crisis resources for you or your loved ones, and best practices for professionals in the United States.
SAMHSA’s National Helpline: 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748(HELP4U) to find help near you. Read more about the HELP4U text messaging service.
NYS OASAS HOPEline: Call 1-877-846-7369 or texting HOPENY (467369) for help and hope 24 hours a day, 365 days a year for alcoholism, drug abuse and problem gambling. NYS OASAS Treatment Availability Dashboard to Search For State Certified Outpatient Or Bedded Programs here.
Jorge R. Petit, MD, is a Behavioral Healthcare Executive Leader. For mor information, visit www.drjpetit.org or email drjpetit@yahoo.com.






