The COVID-19 pandemic has resulted in more than 79 million cases of confirmed infection and over 963,000 deaths in the United States.1 The pandemic has also resulted in increased levels of adverse mental health conditions, substance use and suicidal ideation.2 The reported prevalence of anxiety and depression increased three and four-fold, respectively, over prevalence in 2019.2 Public health measures such as workplace and school closures, physical distancing, forgoing gatherings, testing, and contact tracing have increased isolation and exacerbated existing mental health conditions.
Mental and behavioral health providers have been impacted as well. Researchers from the University of Maryland conducted a survey of 137 mental health providers in the US about how the pandemic has impacted their clients, their services, their own stress and mental health, and what resources they need. Eighty-two percent of respondents reported the pandemic had negatively affected their ability to serve clients and that they are experiencing burnout and fatigue.3 Even before the pandemic, an over-strapped mental health care system has struggled to meet patient demand for services leaving over 100 million people without appropriate access to needed behavioral services.4
Coordinated Behavioral Care (CBC), a not-for-profit organization representing over 60 community-based behavioral health providers in New York City, has been working to help address these unmet behavioral health needs. Through funding from the federal Substance Abuse and Mental Health Services Administration (SAMHSA), CBC has been working with the behavioral health workforce across New York State to understand and address their personal and professional experiences with COVID-19. CBC partnered with Trivedi Consults to design and conduct a survey of their behavioral healthcare providers to identify knowledge, attitudes, and practices related to COVID-19.
Methods
The survey was designed to capture providers’ knowledge and beliefs about the pandemic and the COVID-19 virus, as well as individual and community behaviors, and views and perceptions of COVID-19 vaccination. Responses were collected between February 3, 2021, and February 13, 2021. Approximately 1,585 persons statewide received the survey, 90 completed it, for a 5.7% response rate.
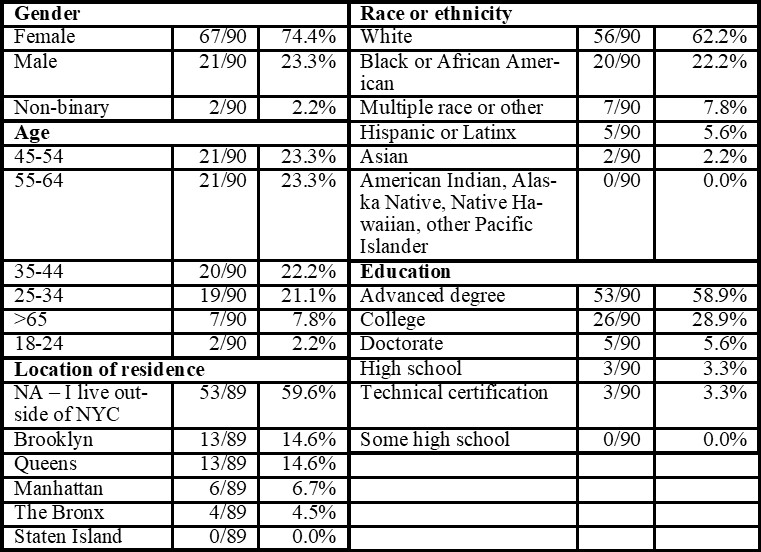
Table 1. Demographics
Results
Respondents were majority female (74%) and diverse in age range. Most respondents live outside of New York City. Sixty-five percent hold an advanced degree or doctorate (see Table 1, Demographics, above).
COVID-19 Prevention Behaviors
Ninety-three percent (84) of respondents reported members of their community wear face coverings and physically distance, and 99% (89) reported that individually they always wear a face covering when entering a public place.
Most respondents were cautious in interactions with people outside their households (see Table 2, Interactions with Others, below). Sixty-three percent (57) reported feeling unsafe getting a drink or meal in an indoor restaurant or bar. Seventy-six percent (68) reported they felt unsafe using the subway. Ninety-four percent (85) reported they would fully participate in contact tracing if diagnosed with COVID-19.
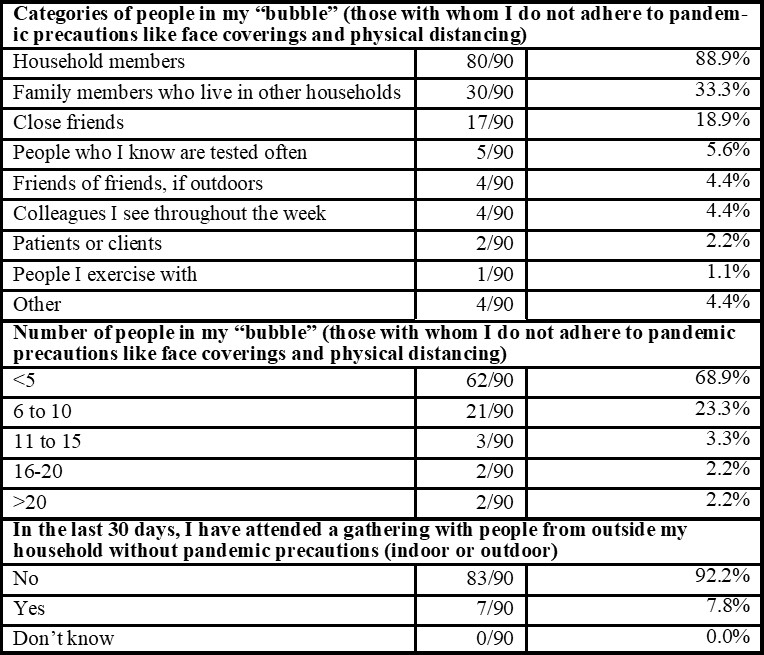
Table 2. Interactions with Others
Discussion
This small survey of behavioral health providers in New York City in February 2021 during the COVID-19 pandemic signals overall capability in seeking and interpreting scientific information. The rates at which respondents selected answers that reflect current scientific understanding of the virus and disease, and the consistency with which they were able to do so across topics, shows frequent engagement with and comprehension of multiple sources of scientific information. For almost all questions that assessed knowledge about COVID-19, transmission, high-risk activities, and vaccination, at least 90% of respondents marked answers that aligned with scientific consensus and current recommendations.
On people’s minds is the question of what should change or improve based on the experience of the COVID-19 pandemic in preparation for “next time,” which is all but assured. For decades, infectious diseases experts have warned of factors that increase the likelihood that society-disrupting pathogens will emerge and spread rapidly widely5 – factors that are all the more prevalent today. In our preparation for the next epidemic or pandemic we should fortify communities by identifying champions for public health and building multidisciplinary partnerships and collaboratives to support and implement public health interventions.
Conclusions
Studies show a high rate of confidence and trust clients have in their behavioral health providers, who also frequently are clients’ main connections to healthcare.6 This survey demonstrates behavioral health professionals’ skills in seeking out scientific sources, keeping up with evolving research and guidance, and interpreting it accurately. Their work is ongoing to guide clients through managing safe behaviors during the COVID-19 pandemic, but as the country considers how to improve the US public health infrastructure and plan ahead, it is important to identify ways to leverage behavioral health specialists’ scientific fluency and trust from clients.
As explained in a recent article from Health Affairs6, efforts should be made to link behavioral health groups to public health agencies both for the purposes of pandemic planning and preparedness for future events, as well as to build vaccine confidence, so that when the “next time” happens, they are ready to serve as a temporary arm of the public health infrastructure. In turn, it is important for organizations such as CBC to continue to remain a trusted resource in providing pandemic information to their members, to remain agile and nimble in pivoting to support the membership during an emergency, and to continue adjusting messaging, training, and information flow based on the latest science and the community’s needs. This survey highlights the critical importance for the development and delivery of needed training for the behavioral health workforce and thereby, their vulnerable clients, to address real-time knowledge gaps particularly important during a pandemic.
Kavita K. Trivedi, MD, is a Physician Epidemiologist and Principal, Valerie Deloney, MBA, is a Science Communications Expert, and Brad Hutton, MPH, is an Epidemiologist at Trivedi Consults. Mark Graham, LCSW, is Senior Vice President, Innovations at Coordinated Behavioral Care. Jorge R. Petit, MD, is the former CEO at Coordinated Behavioral Care and is now CEO at Services for the UnderServed.
For questions, please contact Kavita K. Trivedi, MD at (510) 883-3252, and kavita@trivediconsults.com.
Footnotes
- CDC COVID Data Tracker https://covid.cdc.gov/covid-data-tracker/. Accessed March 16, 2022.
- Czeisler MÉ, Lane RI, Petrosky E, et al. Mental Health, substance use, and suicidal ideation during the Covid-19 Pandemic — United States, June 24–30, 2020. MMWR Morbidity and Mortality Weekly Report. 2020;69(32):1049-1057. doi:10.15585/mmwr.mm6932a1
- Fish JN, Mittal M. Mental Health Providers during COVID-19. Public Health Reports. 2020;136(1):14-17. doi:10.1177/0033354920965266
- New Study Reveals Lack of Access as Root Cause for Mental Health Crisis in America. National Council. https://www.prweb.com/pdfdownload/15828321.pdf. Published October 10, 2018. Accessed May 3, 2021.
- Institute of Medicine (US) Committee on Emerging Microbial Threats to Health, Lederberg J, Shope RE, Oaks SC Jr., eds. Emerging Infections: Microbial Threats to Health in the United States. Washington (DC): National Academies Press (US); 1992.
- Brown JD. To Improve COVID-19 Vaccine Distribution, Engage Behavioral Health Providers. Health Affairs Blog. https://www.healthaffairs.org/do/10.1377/hblog20210128.105637/full/. Published February 2, 2021. Accessed September 14, 2021. doi: 10.1377/hblog20210128.105637







[…] The COVID-19 pandemic has resulted in more than 79 million cases of confirmed infection and over 963,000 deaths in the United States.1 The pandemic has also resulted in increased levels of adverse mental health conditions, substance use and suicidal ideation.2 The reported prevalence of anxiety and depression increased three and four-fold, respectively, over prevalence in 2019.2 Public health measures such as workplace and school closures, physical distancing, forgoing gatherings, testing, and contact tracing have increased isolation and exacerbated existing mental health conditions. Read full article […]